Does the story of Covid-19 in Hawaii reveal a potential murder weapon?
“If I should die before I wake, it’s ‘cause you took my breath away.” Jordin Sparks, ‘No Air’
When considering how severely Covid-19 affected different locations in the United States, Hawaii might be one of the last places to come to mind.
As of 8 March 2023, there have been 1,795 deaths recorded as “Covid-19 deaths” in Hawaii’s official dashboard since February 2020. And while the loss of so many lives is surely upsetting, especially for individuals whose loved ones suffered, the number is small by comparison to other locations of similar size. According to the official state dashboard, only 75 deaths recorded for anyone younger than 40 years old, with 101 deaths occurring for those between 40 and 49.
https://health.hawaii.gov/coronavirusdisease2019/tableau_dashboard/mortality-data/
There were extraordinarily few deaths attributed Covid-19 through spring and early summer of 2020. By 26 July 2020, Hawaii ranked dead last (#50) of all states, according to ( https://247wallst.com/special-report/2020/07/28/states-with-the-highest-number-of-covid-19-cases-18/2/ ) as only 26 deaths had been recorded. This outcome is perhaps unsurprising since reaching Hawaii, consisting of a remote chain of islands in the Pacific Ocean, poses a more difficult journey than other states.
On the other hand, flights between Hawaii and the continental US were routine through 17 March 2020 when Hawaii’s governor, David Ige, announced at a press conference, “I am strongly encouraging our guests to postpone their vacations for at least the next 30 days.” And even then, the announcement was not an outright travel ban. Thus, one might have anticipated that the combination of tourists traveling to Hawaii and residents returning home might have carried the virus to Hawaii through March 2020. (See https://www.hawaiinewsnow.com/2020/03/18/live-governor-discusses-latest-efforts-stem-spread-coronavirus/ )
Despite the lack of rapid transmission of the original Wuhan strain of Covid-19 in spring and summer of 2020, media outlets reported that the delta strain appeared prominently in Hawaii very close to the same time frame that it appeared throughout the rest of the United States. On 6 August 2021 (see https://www.hawaiinewsnow.com/2021/08/06/delta-variant-spreads-hawaii-heres-what-you-need-know-about-virus/ ), Emily Cristobal of Hawaii News Now (HNN) compiled this report, which included an illuminating interview. I believe it is important to provide context to the reader. So for this and many of the most insightful citations in this article, I use bold to emphasize statements which I believe are most essential and to which I may reference later in this article. Here, the entire article is included:
“Hawaii is seeing some of its highest COVID case counts since the start of the pandemic, prompting health officials to urge people to get vaccinated if they haven’t already. The highly transmissible delta variant is being blamed for the record surge in infections.
According to state’s most recent figures, 80% of COVID cases in Hawaii are now the delta mutation. The variant is as contagious as the chickenpox. To understand how the mutation has changed the calculation, HNN spoke to Dr. Tarquin Collis ― Kaiser Permanente’s Chief of Infectious Diseases ― who broke down the impact the virus has on Hawaii and how to mitigate its spread. While health experts are still learning more about the coronavirus and its various strains, the main concern of the delta variant is that it is more transmissible.
“Preliminary science suggests that those who are infected with the delta variant shed more of it when we get sick, we may shed it earlier, and we may shed it for longer.”
He explained that “shedding” refers to the RNA that is shed when you take a nose swab to test for COVID. If you’re shedding a lot of RNA, you’re likely more infectious and shedding more of the virus.
“Early data out of Scotland, Canada and Singapore suggested if you catch delta, you’re more likely to be hospitalized or die than if you had caught an older form of COVID.”
While more research is needed to prove that theory, Collis said COVID mainly manifests in shortness of breath and oxygen levels. In severe cases, other organs — besides the lungs — start to get affected and shut down. This may include kidneys or the heart.
“It can make you sick in ways that are not just about pneumonia. It never fails to amaze me how sick this bug can make you.”
What impact do unvaccinated people have on communities?
“I think it’s never been more dangerous than it is now to be unvaccinated. You have a virus that spreads a lot better than older forms of this virus, you have a virus that might be worse for you. When you work with it day in and day out and you see the difference between taking care of someone who happened to get infected despite vaccination and someone who had not been vaccinated and is profoundly ill — it just breaks your heart as a doctor to see that a lot of lives lost could have been prevented.”
Furthermore, he explained that becoming infected doesn’t only impact your health and the health of those around you, but it can affect your entire way of life.
“There’s a risk to your actual employment by remaining unvaccinated, depending on what you do for a living. And in other states, some are making vaccine passes to enter restaurants and other businesses, which can restrict those who are not vaccinated. That’s a risk to your quality of life as well.”
What’s a “breakthrough” case and should the vaccinated be concerned?
When someone who is fully vaccinated catches COVID, it’s called a “breakthrough” case.
These cases underscore a key point: Vaccines are very effective but can’t offer 100% protection. The very good news is that vaccines are also highly effective in preventing serious illness from COVID.
“It is important to emphasize that breakthrough infections, meaning folks who have been vaccinated and still catch COVID, are almost universally mild. Many of my patients who have been infected after vaccination feel either nothing, and we just pick it up on surveillance, or something that’s closer to a cold or an upper respiratory tract infection.”
He emphasized that more than 90% of hospitalizations at Kaiser are unvaccinated folks, who are filling up emergency rooms and ICU beds.
“Folks who catch this without vaccine protecting them are ending up really, really sick.”
Collis said while it may be a little more likely to become infected with the delta variant compared to prior strains, the vaccine will prevent you from getting super sick.
Do the vaccinated need to take extra precautions now?
Collis explained that even if you are fully vaccinated, it is still important to be vigilant and take precautions depending on who you live with — especially thinking about kupuna, those immunocompromised and children who aren’t old enough to get the vaccine.
“We’re all going to have to come to our own sort of level of comfort as to what makes sense. But I think this would be the time to really think about not going to big indoor events, even if you’re fully vaccinated. I think even crowded outdoor events, if you’re fully vaccinated might be a good idea to wear a mask.”
He encourages “thoughtful masking” and to weigh the risks the virus can have on your life and those you interact with.
“You should always be paying attention to what’s happening around you. Even if you’re fully vaccinated, staying masked still makes sense.”
If you plan on traveling, whether it be for work or to see loved ones, Collis advised to use the best protection when flying in an airplane, such as using N95 masks. He also suggested not eating when everyone else eats or trying to eat before and after the plane ride rather than during the flight.
Why do younger people need to get vaccinated?
Even though data shows that younger populations may not experience as severe COVID symptoms compared to kupuna, Collis said that those infected can still be vectors for the virus.
“If you get infected, maybe it’s OK for you. But you might end up hurting someone that you really care about, who’s older or immunocompromised.”
If a younger person gets infected, they could also still experience lingering effects from COVID.
Hawaii is 60% fully vaccinated. Why are we seeing so many new cases?
While more people are vaccinated compared to the start of the pandemic, Collis explained that COVID is circulating through the population who hasn’t gotten their shots.
“It’s affecting a larger proportion of them because it’s so contagious. When you infect enough people, you’re going to see a ton of people getting sick and ending up in the hospital and the ER.”
He added that the more infectious a virus, the higher percentage of immunity is needed in a population to limit its spread — meaning that more people need to get vaccinated.
Is COVID here to stay?
“As an infectious disease doctor, I think it’s very clear, this virus is going to be with us in the long term. We’ve only eliminated one infectious disease in the history of infectious diseases, and that was smallpox — COVID is no smallpox, this won’t be the second virus that we eliminate by a long stretch.”
He said that COVID has adapted really well to human health and continues to adapt better and better, which is seen in the delta variant.
“For those who think, you know, let me just hang in there and let this thing die down and maybe I’ll never catch it. I think that’s not a strategy that really works.”
What’s the best case scenario for beating COVID?
“My hope is that it settles down ultimately into something that’s more seasonal and more manageable. And that we have a high enough vaccine penetrance that it becomes something closer to the flu, in terms of risk in all of our lives.”
As COVID continues to impact our daily lives, Collis said the number 1 way to fight the virus is to get vaccinated.
“It’s never too late to get the vaccine. For those that are are holding out on vaccination, I would really urge people to reexamine those assumptions and talk with someone that you trust on the medical side about the risks to you and what that represents. COVID is a preventable infection at this point, in terms of severe illness, and these vaccines are quite remarkable. It’s not just for the community, it’s for your own self to really think this through and make a choice — that I think a lot of other people are making — to go for vaccination to get yourself to a safer place.”
Copyright 2021 Hawaii News Now. All rights reserved.
*** Hawaii’s Chris Lederer lost his battle with the virus. ***
The interview was apparently proven prophetic as, only six weeks later, the following story was reported by Honolulu station KHON (Channel 2). This link includes the video of the victim, and excerpts were transcribed in part below: https://www.khon2.com/coronavirus/29-year-old-maui-executive-chef-dies-of-covid
(Anchor) Joe Moore: “Covid has taken the lives of so many people. Last Friday, Chris Lederer lost his battle with the virus. The Maui executive chef had been in the hospital for two months. He was only 29 years old. Jen Boniza spoke to his fiancée (Katrell Mokuahi)…
(Reporter) Jen Boniza: “He (Lederer) and Katrell were engaged to be married in December 2022.”
From article:
COVID-19 has already taken the lives of many. On Friday, Sept. 17 (2021), Chris Lederer lost his battle with the coronavirus. The Maui executive chef was in the hospital since July. His fiancee shared her heartbreaking story and hoped the success he achieved during his life will inspire others. Chris Lederer was passionate about food“He just flowed,” Katrell Mokuahi said. “It was his realm. He started off with Chef Roy (Yamaguchi). And that was straight out of high school.” Mokuahi was Chris’ high school sweetheart — they were engaged to be married in December 2022. Chris was a local boy originally from Paoa. He and Mokuahi moved to Maui several years ago. Chris always dreamed big. “Back in the day, he would always say that, ‘one day I’m going to be big’,” Mokuahi said. “He said that his personal goal was to become an executive chef before he was 30. He did it. He did it,” she said as tears flowed down her face.
He was named the executive chef of The Westin Maui Resort and Spa. Everything went his way until he came down with a cold that turned out to be COVID. Mokuahi took him to the ER on Maui on Wednesday, July 14. “It was a very scary situation. Very scary, very intimidating,” she said.
Chris was intubated a few weeks after he was taken to the hospital, and his condition continued to get worse. But Mokuahi was still able to see him virtually. “The nurses that take care of them are just so amazing,” she said. “They had an iPad that they’re able to set up, prop up to see them. They believe that they’re still able to hear you, and it’s a good healing process to be able to hear the ones that you love. So, I appreciated that so much.”
Despite everyone’s best efforts, Chris’ condition worsened.
“By the grace of God, I was. I was able to be there and talk to him before he passed,” Mokuahi said.
Chris died on Friday, Sept. 17. Mokuahi admitted they were both unvaccinated, but she did not want to push that. “We both were never into politics or vaccinated or unvaccinated,” she explained. “We believe heavily into people having their rights and choices as their own.”
Mokuahi now wants his life to become an inspiration for others. “Dream big, because you never know what you truly could accomplish in this life. You don’t know if tomorrow is going to be there. So why not? You know, why not take the risk?” Katrell Mokuahi, fiancee of Chris Lederer.
She plans to honor his memory by helping other budding chefs get their start.
“He would give the shirt off his back. He has come up from literally the gutter to such an amazing accomplishment of executive chef,” Mokuahi said. “I really do want to start a scholarship in his name, too, to memorialize him, as well as to help others who have the same passion.”
If anyone would like to make a donation to help Lederer’s ohana pay for his funeral arrangements, you can reach out to @honeybubblez or @smash_maui on Instagram. Funeral services and his celebration of life will be announced at a later date.
*** Did oxygen play a role? ***
Chris Lederer’s death occurred after a news story which described conditions in hospitals. One theme was relatively common throughout the United States – that hospital were near capacity. But a second theme – that oxygen supplies were low- was unique to Hawaii:
Published: Sep. 3, 2021 at 10:26 PM EDT|Updated: Sep. 3, 2021 at 11:58 PM EDT
HONOLULU (HawaiiNewsNow) - Hawaii’s health care leaders gave the Senate’s Special Committee on COVID-19 sobering news on Friday about the situation in Hawaii’s intensive care units.
Healthcare Association of Hawaii’s Hilton Raethel told lawmakers every Oahu hospital, except for Tripler Medical Center and Kapiolani Medical Center, is at or near ICU capacity.
The state has 223 licensed adult ICU beds in all of its medical facilities…
As for Hawaii’s liquid oxygen supplies, Raethel said Hawaii will not run short by Sept. 6 ― as had been feared. He said the state is working on getting more oxygen containers and generators, and University of Hawaii engineering professors are helping hospitals find ways to conserve oxygen.
“We have averted the immediate crisis with an incredible amount of work and energy by all parties involved,” he said…
*** Cryogenic oxygen supply limitations in Hawaii ***
The traditional method used for generating oxygen involves cooling air to very low “cryogenic” temperatures at industrials facilities called cryogenic air separation plants, which are operated by companies like AirGas (https://www.airgas.com/resources/gases101/oxygen), Matheson (https://www.mathesongas.com/gases/gas-supply-options/ ), and Air Liquide (https://uk.airliquide.com/gases-and-products/oxygen-o2).
Oxygen, which comprises about 20% of atmospheric air liquefies at temperatures several degrees higher than nitrogen, which comprises almost the remaining 80% of atmospheric air. The trace amounts of argon and other noble gases in the atmosphere also liquefy (or condense) at temperatures lower than oxygen. Through cryogenic refrigeration, fractional distillation may be used to separate oxygen from other gas components of air. Hawaii is remote, so it would have been quite expensive to ship oxygen from other locations in the US, and its liquid oxygen suppliers within the state were faced with demand which outstripped the rate at which they were able to supply the oxygen. For example, see https://www.hawaiinewsnow.com/2021/08/31/hawaii-hospitals-begin-conserving-oxygen-after-influx-covid-patients-strain-states-supply/ published in later August 2021:
“With no sign of Hawaii’s COVID surge leveling out, hospitals are tackling a worrisome new problem: All the extra patients are straining the state’s oxygen supply.
Over the past month, as COVID hospitalizations have grown along with infection counts, daily consumption for medical grade oxygen has jumped 250%, officials say. Hospital leaders held an emergency meeting Monday to discuss ways to conserve the finite resource.
“When resources are scarce we want to ensure that we’re using oxygen appropriately,” said Hilton Raethel, head of the Healthcare Association of Hawaii.
He added oxygen consumption in Hawaii has increased to the point where demand could soon exceed what the state’s two production facilities can supply.
What’s making it even more of a challenge is a worldwide shortage of ISO tanks, the containers needed to transport liquid oxygen via cargo ship.
The state is currently working with the federal government to figure out a solution.
Hawaii Pacific Health President and CEO Ray Vara recently directed staff in an internal memo to conserve the oxygen supply and “avoid using oxygen for anything that is elective.”
“We will therefore need to cancel all elective procedures in operating rooms and elsewhere, including outpatient settings, where oxygen may be needed. Any cases that can be deferred safely should be deferred until the oxygen supply solutions are clearer,” he wrote. “At each HPH facility, surgical and facility leaders will be activating review processes to help with these decisions.”
Lt. Gov. Josh Green said the situation is all the more concerning given that cases continue to soar.
“Going into Labor Day weekend we should be cautious,” said Green, who is encouraging people to avoid gatherings and stay at home over the holiday.
As of Monday, there were 418 people statewide hospitalized with COVID.
Health officials say 88% of them are unvaccinated.
Meanwhile, hospitals continue to deal with staff shortages and help from the mainland is slow to arrive. For the second week in a row, Hawaii welcomed about 40 fewer traveling nurses than expected.
“We have 409 FEMA-funded personnel in the state as of today. And we have another wave coming next weekend,” Raethel said.
He added the state’s two oxygen production sites are operating at full capacity and are now producing medical gas only.
*** Solving the problem of oxygen supply ***
Only a week later, on 7 September 2021, Zoe Dym of Hawaii Public Radio describes the means used by the state to “mitigate an oxygen crisis,” as follows (see https://www.hawaiipublicradio.org/local-news/2021-09-07/how-hawaii-mitigated-an-oxygen-crisis )
How Hawa’ii Mitigated An Oxygen Crisis: Hawaii Public Radio | By Zoe Dym
Published September 7, 2021 at 7:46 AM HST
Last week, almost 100 COVID-19 patients were admitted to intensive care units in hospitals across the state. The surge of COVID-19 patients in hospitals means a higher demand for concentrated oxygen. The state Department of Health previously estimated that Hawaiʻi would run out of oxygen by Labor Day. Several strategies were able to mitigate the crisis.
Two of the oxygen vendors in Hawaiʻi — Matheson and Airgas — switched out the tanks that were used to transport other gases with oxygen. Matheson emptied their argon tank for oxygen, and Airgas donated their nitrogen tanks.
While Matheson and Airgas previously produced commercial grade oxygen, they changed their focus strictly to medical grade oxygen. Production of all other gases are also temporarily on hold. In addition to liquid oxygen from manufacturers, hospitals are supplementing the high demand with oxygen generators. Kaiser Permanente Moanalua Medical Center and Pali Momi Medical Center both installed new generators. Three more federally funded oxygen generators will arrive in Hawaiʻi mid-September.
Chief medical and nursing officers worked with engineering professors from the University of Hawaiʻi to plan oxygen conservation strategies.
Hilton Raethel is the CEO of the Healthcare Association of Hawaiʻi. He says, "We’re working with our hospitals to help them on these oxygen conservation strategies and provide support. That is something that is having an immediate effect or impact in terms of the use of oxygen.
"What this means is that we still provide oxygen as needed. We’re just making sure that we don’t provide more oxygen than what is needed," Raethel explains.
The immediate oxygen crisis has been averted. According to Raethel, Hawaiʻi should not run out of oxygen even if COVID-19 cases continue to increase at its current rate.
*** Mislabeled oxygen tanks… and their perils. History of hospital deaths due to gas mix-up. ***
There are several important points raised in this article. Let’s focus first on the report that oxygen was supplied using “tanks that were used to transport other gases…” Specifically, “Matheson emptied their argon tank for oxygen, and Airgas donated their nitrogen tanks.” While the effort to overcome oxygen supply limitations is admirable, switching tanks increases the likelihood of patients receiving the wrong gas instead of oxygen.
In March 2001, the U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) issued a public health advisory which intended to alert hospitals, nursing homes, and other health care facilities to the hazards of medical gas mix-ups. The Food and Drug Administration (FDA) has received reports during the past 4 years from hospitals and nursing homes involving 7 deaths and 15 injuries to patients who were thought to be receiving medical grade oxygen, but were receiving a different gas (e.g., nitrogen) that had been mistakenly connected to the oxygen supply system. This guidance makes recommendations that will help hospitals, nursing homes, and other health care facilities avoid the tragedies that result from medical gas mix-ups.”
(See https://www.fda.gov/media/70999/download ). The following stories, included in the FDA report, illustrate several occasions where the wrong gas led to patient death and also shows how rare it was for health care workers to catch this mistake:
“On December 7, 2000, a nursing home in Bellbrook, Ohio, reported 2 patient deaths and 8 patients injured following a mix-up in their oxygen supply system. The nursing home had supposedly received a shipment of four cryogenic vessels containing medical grade oxygen. Included in the delivery, however, was a cryogenic vessel of industrial grade nitrogen. The nursing home was running low on oxygen and sent a maintenance employee to connect a new oxygen vessel to the oxygen supply system. The employee selected the nitrogen vessel and discovered, correctly, that he was unable to connect the vessel to the oxygen system — as a safeguard, the connectors for oxygen vessels are specially fitted so they are compatible only with oxygen delivery systems. The employee removed a fitting from an empty oxygen vessel and installed it on the nitrogen vessel. He then connected the deadly product to the oxygen system. Several days later, 2 of the injured patients died from exposure to industrial nitrogen, bringing the death total from this one incident to 4.
On April 22, 1998, a hospital in Idaho discovered that a large cryogenic vessel of industrial nitrogen had been connected to the oxygen system supplying the operating rooms, labor and delivery rooms, and emergency room. The hospital discovered that the medical gas delivery person initially had been unable to connect the incompatible nitrogen vessel outlet fitting to the oxygen system, but had used a wrench to disconnect the nitrogen fitting and replace it with an oxygen fitting. Two patients died as a result of this medical gas mix-up.
In October 1997, a hospital in Nebraska received a shipment of medical grade oxygen in large cryogenic vessels. The shipment included one cryogenic vessel of industrial grade argon that was properly labeled. The hospital was running low on oxygen and sent a maintenance employee to connect an oxygen vessel to the oxygen supply system. Without examining the label, the employee selected the argon vessel, and, discovering he was unable to connect the vessel to the oxygen supply system, he removed a fitting from an empty oxygen vessel, installed it on the argon vessel, and connected the deadly product to the oxygen system. Argon was administered to a patient undergoing minor surgery. The patient died.
On December 2, 1996, a childrens' home located in New York reported adverse reactions experienced by nine patients due to the inhalation of carbon dioxide. An employee of the home, asked to attach a large cryogenic vessel of medical grade oxygen, unknowingly selected a carbon dioxide vessel from the home's inventory. He noted that the fitting on the carbon dioxide vessel was not compatible with the connector on the oxygen system. Nonetheless, he removed an oxygen fitting from an empty vessel, installed it on the carbon dioxide vessel, and attached it to the oxygen supply system. Two patients were injured critically, and four patients experienced varying stages of respiratory distress.
…many medical gases are improperly or poorly labeled; the wrong gases are delivered accidentally to hospitals, nursing homes, and other health care facilities; and poorly trained personnel are connecting the wrong vessels to oxygen supply systems, despite connection incompatibilities. Patients continue to suffer injury or death.
Other reports of gases being mixed up with oxygen are readily available through internet searches. Some examples are as follows:
https://www.nytimes.com/1983/05/29/us/army-finds-welding-gas-brought-hospital-deaths.html
FORT McCLELLAN, Ala., May 28, 1983 (AP) - A tank resembling an oxygen container but faintly labeled ''argon,'' a gas used in welding, was examined by investigators today after the deaths of two patients who breathed the gas at the Army hospital here.
Military officials confirmed early today that two patients died and a third lapsed into a coma Wednesday because the argon tank was connected to the main oxygen supply system at Noble Army Hospital on Fort McClellan in Anniston.
The 100-bed hospital's operating and delivery rooms had been closed for three days while investigators determined what killed a sergeant and a premature infant and left the wife of another Army sergeant near death.
''It is apparent that we were supplied argon in place of oxygen in a tank normally used for oxygen,'' said Col. Edward M. Johnson, a doctor and the commander at the hospital. ''Subsequent administration of argon to the patients resulted in suffocation.''
Odorless and Nontoxic
Colonel Johnson said argon, a colorless, odorless and nontoxic gas primarily used in welding, was in one of two tanks that supplies the major source of oxygen for the hospital's emergency room, operating rooms, the delivery and labor room and the nursery, as well as several wards and clinics.
The hospital contracted with Dixie Welding Supply of Attalla for the oxygen, but discontinued ordering from the company on Thursday, Colonel Johnson said.
NORRISTOWN, Pa., Aug. 2, 1977 - The apparent switching of labels on oxygen and nitrous oxide outlets in a hospital emergency room was responsible for several deaths, the administrator of the hospital said today.
Pennsylvania's Department of Health opened an investigation today into the error at Suburban General Hospital in an effort to determine how many deaths may have been caused by the blunder.
Richard B. Anderson, administrator of the 141‐bed osteopathic hospital in East Norriton Township, said the toll attributable to the mixup would prove to be no higher than five. In the six months before the mislabeling was discovered on July 6, 35 deaths were recorded in the new emergency room.
Mr. Anderson blamed an “inadvertent mechanical error” by the general contractor and a subcontractor for the misplacing of the color‐coded labels.
Sadly, more recent examples are also easy to find.
From Italy, as reported by The Guardian in May 2007: https://www.theguardian.com/world/2007/may/07/italy.international
“A face mask which emitted massive and fatal doses of anaesthetic gas instead of oxygen has been blamed for the sudden death of a 73-year-old patient at an Italian coronary unit and is suspected to have killed another seven patients at the unit since it opened 17 days ago.
Doctors at Castellaneta hospital in Puglia admitted that the tubes supplying oxygen and anaesthetic gas to the ward had been switched in error, causing the death on Friday of Cosima Ancona, who was being treated for a minor heart arrhythmia.
Investigators will now start autopsies on patients who died in the ward and are mounting a multiple manslaughter inquiry.”
And from ABC Australia in 2016: https://www.abc.net.au/news/2016-09-06/hospital-gas-mix-up-parents-of-baby-devastated/7816858
“The parents of a baby girl who suffered permanent brain damage when she was accidentally administered laughing gas at a Sydney hospital say she is experiencing constant seizures and must be fed through a tube. Baby Amelia Khan was inadvertently given nitrous oxide instead of oxygen shortly after she was born at Bankstown-Lidcombe Hospital in Sydney's southwest on 20 June 2016.
Her parents, Benish and Danial Khan, said Amelia was a much anticipated first child and they were devastated the incident had left her with irreversible brain damage. We remain full of hope for Amelia's future but we worry for her and want to do everything we can to make sure she has the best life she possibly can," they said in a statement.
A month after Amelia was born, a second baby born at the same hospital was also given nitrous oxide and later died.
Mr and Mrs Khan have expressed their sympathy to the parents of the baby boy…”
*** Did Chris Lederer die of a “switching of tanks” which caused him to be supplied nitrogen or argon instead of oxygen? ***
We know that Covid-19 very rarely leads to death among young people without serious pre-existing conditions. Chris Lederer was healthy, employed as an executive chef, and was only 29 years old when he died. Is it possible that Chris Lederer’s death was attributable to a “switching of tanks” which caused him to be supplied nitrogen or argon instead of oxygen? For example, suppose a vessel of properly-labeled nitrogen at the manufacturing facility were mistakenly assumed to be a tank of oxygen and shipped to the hospital. If the staff at the hospital were subsequently told to be unconcerned about the label - that the container actually contained oxygen, the staff may have mistakenly supplied nitrogen instead of oxygen to patients. Health-care workers then might have assumed that a patient, such as Chris Lederer, was struggling and ultimately died solely due to the effect of Covid-19 on his lungs. Has the possibility that Chris Lederer died of an oxygen gas mix-up been carefully investigated?
Moreover, three pregnant women died in Hawaii over the course of only 5 weeks in September-October 2021. Given the circumstances of their deaths, is it possible that one or more of them died as a result of being provided a gas to breathe which was not oxygen? Here are their stories:
*** 14 September 2021 – First Covid-19 death for a pregnant mother in Hawaii reported ***
HONOLULU (HawaiiNewsNow) - Doctors have confirmed a pregnant woman in the islands who was severely ill and hospitalized with COVID recently died after giving birth, in a tragic first for Hawaii.
In the wake of the fatality, health officials are urging pregnant women to get vaccinated.
“We have been notified of a maternal death ― so a mother who died postpartum after giving birth,” said Dr. Stacy Tsai, chair of Hawaii State Maternal Mortality Review Committee. “The baby was delivered and is doing fine. The mother unfortunately had very severe disease from COVID.”
Due to medical privacy, Tsai says she can’t publicly share many details about the case or the mother’s vaccination status. But she did say the loss impacts everyone. “It is very devastating. It’s an infant or newborn who will never really know its mother and will never experience the love of a mother,” said Tsai.
“Me and my team, we grieve every day when we have a bad outcome,” she added.
The CDC says pregnant and recently pregnant women are more likely to get severely ill from COVID-19.
“We are seeing women getting COVID during pregnancy and becoming so sick that we are having to deliver pre-term or premature in order to help them breathe, unfortunately, better,” said Tsai.
On the Papa Ola Lokahi Facebook page recently, Native Hawaiian physicians held a webinar about wahine health, pregnancy and vaccine safety.
The recent death was part of the discussion.
“All of the women who have been hospitalized during pregnancy have been unvaccinated,” said Dr. Reni Soon, OB/GYN at University Health Partners and a JABSOM associate professor.
“I’ve been an OBGYN for 20 years here in Hawaii. I’ve seen more pregnant women intubated and on ventilators in the last two months than all the rest of my years,” Leading medical organizations agree the vaccine is safe for pregnant women. “Get vaccinated if you are pregnant,” Tsai said. Get vaccinated if you are around people who are pregnant.”
The American College of Obstetricians and Gynecologists has a Q&A on its website about the vaccine and pregnancy. You can also find more information on the CDC’s website.
*** 20 September 2021 – Second Covid-19 death for a pregnant mother in Hawaii reported ***
https://www.khon2.com/coronavirus/second-pregnant-hawaii-woman-dies-of-covid-19/
HONOLULU (KHON2) — The COVID-19 virus claimed the lives of two pregnant women in Hawaii during the month of September.
“We had our second maternal deaths from COVID recently, and these are moms who actually contracted the disease when they were pregnant, and then deliver their baby and subsequently pass away from COVID-19,” explained Dr. Stacy Tsai, chair of the Hawaii State Maternal Mortality Review Committee.
She said both babies were doing okay.
She could not disclose much information for privacy reasons but said both women were severely ill.
“We haven’t had to really intubate anybody, or put breathing tubes in with the alpha strain, so the delta variant is affecting our pregnant moms, I think more severely,” Dr. Tsai said.
She said pregnant women have a higher risk of being on a ventilator, in the ICU and dying than non-pregnant women who contract COVID.
“We are seeing higher rates of women either going into labor early or actually having to be induced early because their disease is so severe, and they can’t breathe, right? When you can’t breathe, you’re also not giving your baby oxygen,” Dr. Tsai also explained.
The CDC recommended pregnant women get the vaccine in April after studies showed no obvious safety concerns for 35,000 women and their babies.
“We are not seeing an increased risk of complications, we’re not seeing an increased risk of miscarriages, birth defects or really any complication,” she continued.
“Your immune response actually could cross the placenta and actually help the baby,” Dr. Tsai added. “And the protective immunity actually goes through your breast milk so when you’re breastfeeding the baby, it actually give the baby immunity against COVID-19.”
She suggests pregnant women should talk with their doctors if they have any concerns about the vaccine.
“When a mom dies, the entire community and the entire family suffers,” Dr. Tsai said, “and I really, really, really want to prevent future deaths, maternal deaths from COVID-19, and I think the answer is to get everybody vaccinated.”
*** 21 October 2021 Third Covid-19 death for a pregnant mother in Hawaii reported ***
A third maternal death due to COVID-19 in Hawaii has been confirmed, according to the committee that oversees them.
Dr. Stacy Tsai, chair of the Hawaii Maternal Mortality Review Committee, confirmed that a third pregnant woman has died from the coronavirus after giving birth. Her baby survived.
Two other maternal deaths occurred in September among women who suffered from severe disease due to the coronavirus. They also died after giving birth, and their babies also survived. The news comes as Hawaii doctors urge pregnant and recently pregnant women to get vaccinated due to high risks from contracting COVID-19.
Women who are pregnant and recently pregnant are at an increased risk for severe illness from COVID-19, according to the Centers for Disease Control and Prevention, requiring hospitalization, intensive care or ventilators. Additionally, pregnant women who contract the virus are at increased risk for preterm birth and other adverse pregnancy outcomes, including stillbirth.
The CDC recently issued an urgent health advisory on the need to increase vaccination rates among pregnant and recently pregnant women, saying the benefits outweigh known or potential risks.
Further, doctors advise that pregnant women receive a booster COVID-19 shot if it’s at least six months since they became fully vaccinated.
Only about 34% of women ages 18 to 49 who are pregnant in the U.S. have been vaccinated, according to statistics released in mid-October — compared to about 25% in August.
The Hawaii Department of Health has reached out to the community via social media channels, urging pregnant women to get vaccinated in light of CDC’s findings. “We recommend all people who are pregnant, breastfeeding or thinking about becoming pregnant get vaccinated against COVID-19,” said the DOH in a Facebook post. “Protect your child and yourself by getting vaccinated. Increased risk of severe illness and pregnancy complications related to COVID-19 infection make vaccination more urgent than ever.”
Health Director Dr. Elizabeth Char is also urging this demographic to get vaccinated against COVID-19.
“We urge expectant moms and those planning to get pregnant to get vaccinated,” said Dr. Char in a statement. “The vaccines are both safe and effective for pregnant women. Research shows the vaccines do not increase the risk of miscarriage. Instead, they protect women from serious complications associated with COVID-19.”
*** Is ‘privacy’ being invoked to protect hospitals from liability? ***
It seems advisable for family members of the deceased women to seek an advocate to investigate whether oxygen might have been substituted for a different gas. Certainly, if a hospital made a mistake which led to a pregnant woman’s death, a court would be disposed to hold them liable for damages. If such a circumstance arose for any of the three women, the newborn baby suffered more than anyone and is entitled to compensation.
However, none of the three stories include the name of any of the women. Likewise, a web search yielded no news stories or obituaries about the three women. This seems odd to me, given that there is no shame associated with dying of Covid-19. Moreover, Hawaii has a rather modest population compared to other state. In September, state records show there were a total of 1276 deaths while October had 1146. Similarly, the number of births in each month was only between 1300 and 1400. Why wasn’t this bigger news in Hawaii?
https://health.hawaii.gov/vitalstatistics/preliminary-vital-statistics-for-2021/
One might anticipate that social media outlets would have circulated the news about at least one of the three women, perhaps to assist the family with the expenses and emotional support for a baby born unexpectedly without his or her own mother under such tragic circumstances. Why would that be so difficult to find? Why wouldn’t people in her community talk about her tragic story?
Naturally, privacy is important. Yet consider the remark above by Dr. Tarquin Collis in his interview, “And in other states, some are making vaccine passes to enter restaurants and other businesses, which can restrict those who are not vaccinated. That’s a risk to your quality of life as well.”
Clearly, there is a public interest in knowing whether a hospital has administered the wrong gas to patients and caused their deaths. By contrast, there is no reason apart from imposition of power for a restaurant to require a patron to disclose of a person’s vaccination record.
It is also interesting that the news stories fail to include the name of the hospitals in which the patients died. By any chance, was it the same hospital for all three of the women? Or is the hospital’s name also protected for sake of ‘medical privacy’? Hospital administrators would certainly advocate for such ‘privacy’ since their hospitals might be subjected to massive lawsuits if their actions led to a patient’s death.
It seems that the medical privacy of the patients was breached by Dr. Remi Soon, who noted that “All of the women who have been hospitalized during pregnancy have been unvaccinated,” said Dr. Reni Soon, OB/GYN at University Health Partners and a JABSOM associate professor.
It is only natural to conclude that the three women who died were unvaccinated since they died at the hospital. Has Professor Remi Soon been censured for this, perhaps inadvertent, disclosure?
Dr. Soon also says that, “I’ve been an OBGYN for 20 years here in Hawaii. I’ve seen more pregnant women intubated and on ventilators in the last two months than all the rest of my years.”
In which hospital or hospitals did Dr. Soon witness the women who were intubated? Is it possible that all of the pregnant women who were struggling to breathe were being supplied a gas other than oxygen?
According to https://fpfellowshiphawaii.org/faculty/reni-soon-md-mph/ , Dr. Remi Soon is the Co-director of Complex Family Planning Fellowship Program. Her interests include “Pregnancy Intention and Contraception Use among Native Hawaiian Women, Reproductive Health Advocacy, and
Reproductive Justice.” Given her interest in contraception and family planning, how many pregnant women does Dr. Soon typically see over a two-month period of time?
Is it possible that social media has been silent due to the women being in a compromised situation? For example, were any of the three expectant mothers single and in the United States illegally? If they had no family in Hawaii to advocate for them, then who would advocate for their three newborn children? For the sake of the babies born under such tragic circumstances, I plead for openness and transparency regarding the names and circumstances of the three women who perished. Perhaps family or friends of the women might set up a legal fund to discover whether or not the wrong gas was supplied to their loved one. At a minimum, the public should know the name of the hospital(s) which cared for the three women.
*** Oxygen Gas Generators: A new technology ***
The article by Zoe Dym also discusses another important point, repeated as follows: “In addition to liquid oxygen from manufacturers, hospitals are supplementing the high demand with oxygen generators. Kaiser Permanente Moanalua Medical Center and Pali Momi Medical Center both installed new generators. Three more federally funded oxygen generators will arrive in Hawaiʻi mid-September.” Therefore, it is conceivable that the Hawaiian hospital which cared for Chris Lederer did not use cryogenic oxygen sourced from a supplier but rather utilized an oxygen generator.
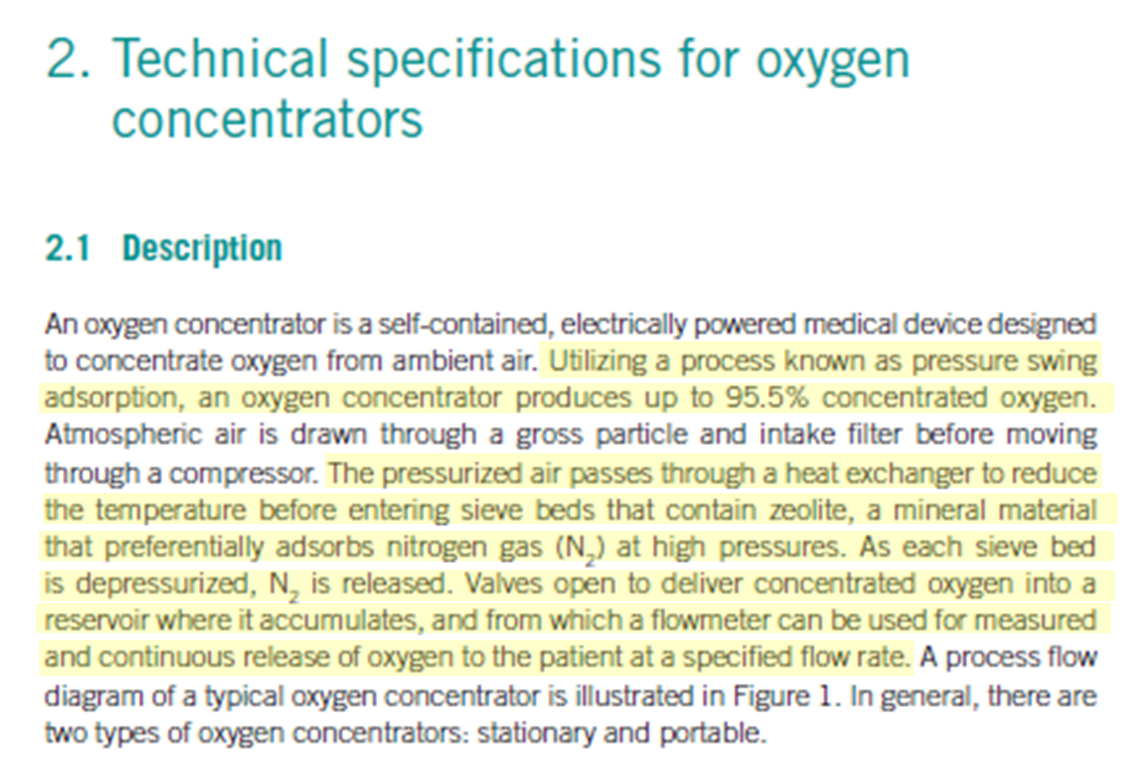
Oxygen generators have become economically viable in recent years through technological development of ‘pressure swing adsorption.’ An excellent recent review of adsorption processes using zeolites is given by Perez-Botella, Valencia and Rey in the academic journal “Chemical Reviews” at ( https://pubs.acs.org/doi/pdf/10.1021/acs.chemrev.2c00140 ). The authors describe zeolites as “crystalline microporous aluminosilicates” which have a “well-defined pore size, compositional tunability, thermal stability and commercial availability since the 1950s.”
The authors continue: “The term zeolite was coined by Swedish mineralogist Axel F. Cronstedt in 1756 when he saw froth forming on the surface of a mineral sample up one heating. The mineral was apparently ‘boiling’, and thus he named is ‘zeolite’, from the Greek zein ‘to boil’ and lithos ‘stone’. Later, this phenomena was ascribed to the presence of hydration water inside of the pores of the mineral, which is liberated upon heating.” Later, in 1840, it was found that the process could be used in a reversible process. In other words, the zeolite could be hydrated to store water and then dehydrated to release it. This property is why zeolite materials are presently used as water softeners, according to the authors, for some laundry applications.
Zeolitic adsorbents can be synthesized for industrial uses which go far beyond storage and release of water. According to Perez-Botella et al., “The most important property of zeolites, and the one on which their applicability as catalysts, adsorbents, and ion exchanges depends, is their structural porosity. Closely related to this feature, their narrow pore size distribution makes them useful for applications in which size and shape selectivity are involved.”
The authors continue: “Adsorption is defined as the enrichment in the concentration of molecules, atoms, or ions present in a fluid (either liquid or gas) phase in the vicinity of an interface. In the case of a solid-gas system, this interface is the surface of the solid… The use of zeolites as adsorbents stems ultimately from their microporosity and regular pore size.”
In 1932 J.W. McBain coined the term “molecular sieve” recognizing that if porosity size and distribution of zeolites could be controlled during manufacturing of the material, specific molecules could be separated from a mixture. For example, a properly fabricated zeolite adsorbent could adsorb oxygen while nitrogen and the remaining components of air would not be adsorbed, thus achieving the goal of separating nitrogen from oxygen. Of course, this posed a tremendous challenge because oxygen and nitrogen molecules are of a similar size.
Decades of research and development were invested into synthesizing zeolites with the proper structural porosity in order to adsorb nitrogen but not oxygen. In addition to size, Perez-Botilla et al. report that: “The interactions of the quadrupole of nitrogen with the cations are considered the basis of the selectivity of these adsorbents.” In other words, early designs of oxygen gas separation via zeolite adsorption were carried out by adsorbing nitrogen and while oxygen flows out as the desired product. (In more recent years, zeolite synthesis technology has matured to the point to which adsorbing oxygen from air become practical.)
There is a second step to the separation process especially pertinent to oxygen generators. Perez-Botella et al. continue: “Industrial gas adsorption processes use a technology named ‘swing adsorption’ in which the adsorbent bed is subjected to cycling conditions of pressure or temperature, thus giving rise to pressure swing adsorption or temperature swing adsorption. Pressure swing adsorption is mostly used in bulk separations, where the component to be separated represents more than ten percent of the stream to be processed… Pressure swing adsorption technology was (initially) developed in the 1960s” and meant a great breakthrough, as it promoted research on adsorption processes and new adsorbents.”
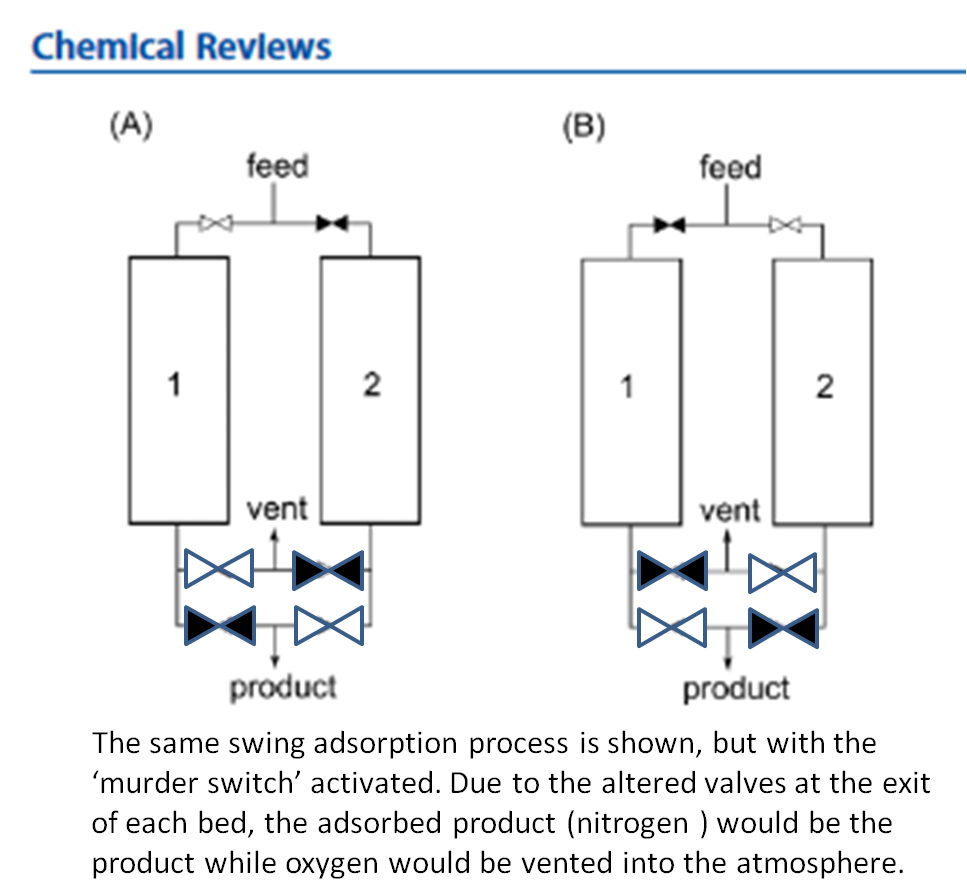
“The conceptual scheme of a pressure swing adsorption process is relatively simple (see figure below).
A minimum of two adsorbent beds in parallel are necessary. Taking the case of just two beds, the stream to be purified flows through bed number 1 which has just been regenerated and is activated and ready to adsorb. Meanwhile, bed number 2 is being regenerated by either decreasing pressure or increasing temperature.”
The figure represents a process in which nitrogen is the gas adsorbed. First consider the image labelled (A) on the left. Pressurized air flows into the zeolite bed, and nitrogen is adsorbed while oxygen flows out as the desired product. The valve to Bed number 2 is closed, so no air flows into it. Rather, the temperature in Bed 2 is raised to allow the desorption of nitrogen from the zeolite. For Bed number 2, the valve is open as indicated by the color white, as stated in the figure’s caption, to the vent, rather than the product. So nitrogen, previously adsorbed by the zeolite, is simply released back into the atmosphere as it desorbs from the zeolite when the temperature of the bed is raised. Thus, it is said that Bed number 2 undergoes “regeneration”. After the nitrogen has been vented for a long enough time, it is prepared to adsorb more nitrogen.
The right image, labelled (B), represents a later time within one cycle, at which the valve to the high pressure air is closed (as indicated by its black color) for Bed number 1 while a separate valve to the high pressure air is open at the inlet of Bed number 2. Under this condition, the zeolite in Bed number 2 adsorbs the nitrogen while oxygen flows through an open valve (shown in white) into a tank as the desired product. Meanwhile, Bed number 1, with zeolite initially saturated with nitrogen undergoes the regeneration step as nitrogen is vented to the atmosphere.
This second step completes the cycle, valves are returned to their position shown in (A), and another cycle is initiated. The cycling is repeated over and over again, which leads to the descriptor ‘pressure swing’ since the high pressure air ‘swings’ back and forth to each bed with the adsorbent material after regeneration of the zeolite. Each bed ultimately supplies the desired product, oxygen, when the process functions properly.
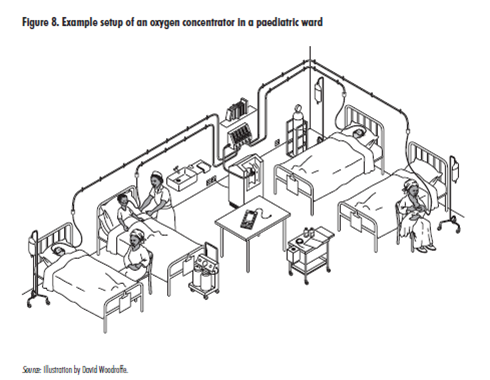
The same zeolite bed adsorption technology for oxygen separation is used for smaller-scale units called ‘oxygen concentrators,’ which are described in this World Health Organization (WHO) document titled, “Technical Specifications for Oxygen Concentrators,” referenced as ISBN 978 92 4 150988 6, and copyrighted in 2015.
http://apps.who.int/iris/rest/bitstreams/887042/retrieve
This document describes the same pressure swing process using zeolite beds, represented in the figure by Perez-Botella, along with a few additional details, as seen in the accompanying excerpt and schematic.
While oxygen gas generators can supply oxygen for large facilities, such as hospitals, oxygen concentrators are sized to supply either individual patients or a small group, as shown in the next figure from the same WHO document.
The WHO document’s acknowledge section includes the following statement: “This document builds primarily on the outcomes of a meeting of subject matter experts in oxygen concentrators, organized by PATH and Bill & Melinda Gates Foundation in Seattle on 13-14 August 2014.”
This document builds primarily on the outcomes of a meeting of subject-matter experts in oxygen concentrators, organized by PATH and the Bill & Melinda Gates Foundation in Seattle on 13–14 August 2014. The goal of this expert advisory group meeting was to build consensus on approaches to improve oxygen concentrators to treat paediatric patients with hypoxaemia or severe respiratory distress in low-resource settings (LRS). The meeting identified several key issues related to technical specifications for oxygen concentrator equipment, including procurement, performance and maintenance. ]
This statement is also shown in context below, which also acknowledges the contributions of the World Health Organization (WHO) and PATH. PATH is a non-governmental organization which was founded in 1977 as the Program for the Introduction and Adaption of Contraceptive Technology with a focus on ‘family planning’.
*** The PATH to India ***
Thus, it is unsurprising that PATH and the Gates Foundation would be involved in providing oxygen generators to health facilities throughout the world.
For example, this story was published on 21 May 2021 regarding India (emphasis added using bold font).
https://www.geekwire.com/2021/gates-foundation-seattle-nonprofit-path-helping-get-oxygen-india/
“The Bill & Melinda Gates Foundation has teamed with two Chicago financial groups to channel $5.5 million into efforts by Seattle-based nonprofit PATH to bring more oxygen to COVID-19 patients in India.
“Lack of access to medical oxygen is one of the defining health challenges of our age,” said Chris Elias, president of global development at the Gates Foundation. “As we are now seeing in India, the consequences can be dire.” PATH is working with officials in 10 Indian states to help identify sources of oxygen for hospitals. PATH teams also are helping agencies identify how much oxygen local hospitals have on hand, and how much they’re going to need.
India is being overwhelmed by a second-wave COVID crisis that is killing more than 4,000 people a day. The official death toll was 262,000 as of Thursday, according to Johns Hopkins University. But the Institute for Health Metrics and Evaluation at the University of Washington has warned that the actual number of deaths is probably three times that. IHME projects total COVID deaths in India will top 1 million by Aug. 1. Lack of medical oxygen in hospitals is compounding the crisis in India. Hospitals in many areas report running low or even completely out of oxygen on a regular basis. So many people are dying that cemeteries and crematoriums in some areas can’t keep up. The problem is that COVID patients require far more oxygen than hospitals would use on a patient with another disease, said Mohammed Ameel, PATH’s head of primary healthcare, technology and innovations in New Delhi. Oxygen is particularly important to seriously ill COVID patients, who usually develop pneumonia.
About 15% of COVID patients in India require oxygen, Ameel said. According to one report, major Indian hospitals are now using as much oxygen each day as they normally would in a week.
Under typical circumstances, India produces more than enough oxygen to meet its medical and industrial needs, Ameel said. But as demand has increased, the country’s supply chain has broken down. Large rail tankers that bring liquid oxygen to major hospitals used to travel 200 kilometers from production site to delivery point; now they’re traveling 1,000 kilometers to bring emergency oxygen to new customers, he said.
“The challenge is supply chain and turnaround time,” Ameel said.
And not all hospitals have the capacity to handle the huge oxygen tanks, Ameel said. “The challenge is not only in production, but if you produce enough, how do you transport that, and when you get to the hospital, where do you store that?” he said. “(In many cases) you don’t have the capacity to do that.”
PATH has been working closely with officials in the states of Punjab, Maharashtra and Karnataka to help them address those issues. Karnataka’s capital is the tech center of Bengaluru, also known as Bangalore; Maharashtra’s capital is Mumbai, the nation’s financial center. “We’re supporting procurement,” Ameel said. “We’re helping them securing oxygen concentrators and oxygen generator plants.”
Building new oxygen generator plants closer to hospitals cuts down logistical problems. And oxygen concentrators — small, bedside units that pull in air, remove the nitrogen, carbon dioxide and other gases — can provide oxygen for a handful of patients. Oxygen concentrators are particularly helpful in areas where hospitals are full, Ameel said, because patients can be sent home with one.
Donations like the one from the Gates Foundation have been pouring in in response to the crisis in India, said Carla Sandine, PATH’s chief of external affairs.
“We are seeing an outpouring of support across the United States for the global COVID crisis,” she said. “That includes the U.S. government and it includes U.S. companies.”
Last year, donors were focused on giving to domestic COVID relief efforts, she said. But now “I feel a shift,” Sandine said. “In the U.S., people are feeling relieved about what’s starting to happen here and horrified that much of the world has no end in sight.” And, she noted, in places like Seattle, “the Indian diaspora is large and engaged and charitable and beloved.”
Last week Seattle-area tech leaders formed a group called Seattle for India that’s trying to raise $10 million to support efforts that are delivering crucial healthcare supplies to India. Hometown tech giant Microsoft is also lending a hand, using its technology and donations to help the cause.
PATH is using donations in two primary ways, Sandine said: providing funding to deploy teams and resources to India and adjacent countries to scale up oxygen production, and to help fund development and testing of a new low-cost COVID vaccine that could be manufactured in many places worldwide.
The Gates Foundation teamed with Chicago-based Citadel, an investment management firm, and Citadel Securities, a finance company, to make the donation. It’s the first announced grant since Bill and Melinda Gates announced plans to divorce on May 4.”
May. 7, 2021, 12:00 PM
CHICAGO, May 7, 2021- The partners of Citadel and Citadel Securities today announced new commitments totaling $5.5 million to increase the supply of medical oxygen in India. As the nation experiences a devastating surge in COVID-19 cases, the demand for medical oxygen has risen to unprecedented levels.
The grants from Citadel and Citadel Securities, the Bill & Melinda Gates Foundation and Gates Philanthropy Partners have been directed to the global health nonprofit PATH. They will be used to support near-term, critical needs while also building infrastructure that will be beneficial far beyond the current pandemic.
"Our hearts go out to the people of India as they battle this devastating surge in COVID-19," said Ken Griffin, Founder and CEO of Citadel. "We are proud to continue accelerating impactful solutions to address urgent needs during the pandemic."
"Lack of access to medical oxygen is one of the defining health challenges of our age," said Chris Elias, President of Global Development at the Bill & Melinda Gates Foundation. "As we are now seeing in India, the consequences can be dire, which is why we must come together with others to help address this important issue both during the current crisis and beyond."
Citadel and the Gates Foundation have partnered with PATH, an organization that works with governments, businesses and other organizations to solve the world's most pressing health challenges. PATH is currently coordinating with multiple state governments in India to address the oxygen shortage, while also providing the technical expertise required to set up oxygen-generating plants at healthcare facilities.
"PATH is responding to the urgent COVID-19 crisis in India and globally, including monitoring medical oxygen demand, increasing access to vaccines and strengthening disease surveillance," said Nikolaj Gilbert, President and CEO of PATH. "Our impact hinges on the generosity of our partners. We are grateful for the support Citadel and the Bill & Melinda Gates Foundation have shown so that we can continue our lifesaving work where it is needed most."
***
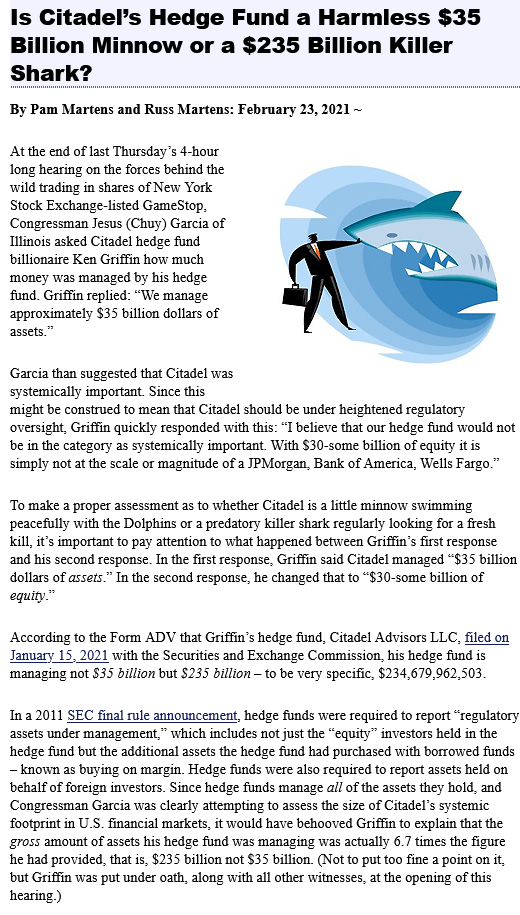
It turns out that the $5.5 million gift by Citadel and Citadel Securities in May 2021 came fewer than three months after founder and CEO Ken Griffin testified to Congress regarding its role in the GameStop-Robinhood scandal. The details of the scandal are beyond the scope of the present discussion, but it is relevant to consider the motivation for Citadel to choose to make this specific philanthropic gift.
Statements by CEO Griffin during his sworn testimony were characterized as false and/or misleading in the two articles published by wallstreetonparade.com below.
https://wallstreetonparade.com/2021/02/gamestop-hearing-citadels-ken-griffin-doesnt-let-the-brutal-facts-get-in-the-way-of-his-testimony/ (By Pam Martens and Russ Martens: February 18, 2021)
“The billionaire hedge fund titan of Citadel LLC and its market-making/trade execution arm, Citadel Securities, delivered a load of horse pukky in his written testimony to the House Financial Services Committee…
...Citadel Securities is majority-owned by Griffin and was the unit executing trades for Robinhood’s retail customers in an arrangement known as payment-for-order flow. According to Wall Street’s self-regulator, FINRA, which keeps track of fines and alleged wrongdoing by all regulators, Citadel Securities has been fined and/or censured 59 times in the past 12 years. If a retail broker had Citadel Securities’ history of fines and alleged transgressions by regulators, he would have long ago been barred from working in the industry.
In some cases, the allegations against Citadel Securities are mind-numbing in terms of quantity and the span of time over which they occurred. Here’s a small sampling:
On July 16, 2020, Citadel Securities agreed to a $700,000 fine by FINRA for executing customer orders at prices worse than it traded for its own account. It was allowed to neither admit nor deny the charges. The activities did not occur over a matter of days or weeks – but over a period of years…”
***
The second article, published shortly afterward, was more pointed in dissecting the testimony.
Is Citadel’s Hedge Fund a Harmless $35 Billion Minnow or a $235 Billion Killer Shark?
By Pam Martens and Russ Martens: February 23, 2021
“At the end of last Thursday’s 4-hour long hearing on the forces behind the wild trading in shares of New York Stock Exchange-listed GameStop, Congressman Jesus (Chuy) Garcia of Illinois asked Citadel hedge fund billionaire Ken Griffin how much money was managed by his hedge fund. Griffin replied: “We manage approximately $35 billion dollars of assets.”
Garcia then suggested that Citadel was systemically important. Since this might be construed to mean that Citadel should be under heightened regulatory oversight, Griffin quickly responded with this: ‘I believe that our hedge fund would not be in the category as systemically important. With $30-some billion of equity it is simply not at the scale or magnitude of a JPMorgan, Bank of America, Wells Fargo.’
To make a proper assessment as to whether Citadel is a little minnow swimming peacefully with the Dolphins or a predatory killer shark regularly looking for a fresh kill, it’s important to pay attention to what happened between Griffin’s first response and his second response. In the first response, Griffin said Citadel managed “$35 billion dollars of assets.” In the second response, he changed that to “$30-some billion of equity.”
According to the Form ADV that Griffin’s hedge fund, Citadel Advisors LLC, filed on January 15, 2021 with the Securities and Exchange Commission, his hedge fund is managing not $35 billion but $235 billion – to be very specific, $234,679,962,503.
In a 2011 SEC final rule announcement, hedge funds were required to report ‘regulatory assets under management,’ which includes not just the ‘equity’ investors held in the hedge fund but the additional assets the hedge fund had purchased with borrowed funds – known as buying on margin. Hedge funds were also required to report assets held on behalf of foreign investors. Since hedge funds manage all of the assets they hold, and Congressman Garcia was clearly attempting to assess the size of Citadel’s systemic footprint in U.S. financial markets, it would have behooved Griffin to explain that the gross amount of assets his hedge fund was managing was actually 6.7 times the figure he had provided, that is, $235 billion not $35 billion. (Not to put too fine a point on it, but Griffin was put under oath, along with all other witnesses, at the opening of this hearing.)
Citadel’s hedge fund consists of a series of sub-funds that have varying investment strategies and asset classes including stocks, bonds and commodities. A Citadel hedge fund brochure that is also on file with the SEC explains how leverage is piled on: “The sub-funds generally invest on a highly leveraged basis, and the Funds may leverage their investments in the underlying sub-funds.”
According to Citadel’s Form ADV, a majority of its sub-funds that hold the largest amount of gross assets are organized in the Cayman Islands, a jurisdiction prized for its secrecy. Those include: Citadel Multi-Strategy Equities Master Fund Ltd. with $59 billion in gross assets; Citadel Equity Fund Ltd. with $25.7 billion in gross assets; Citadel Kensington Global Strategies Fund Ltd. with $17.3 billion in gross assets; and Citadel Quantitative Strategies Master Fund Ltd. with $8.3 billion in gross assets.
The SEC’s Form ADV asks the question: “What is the approximate amount of your total regulatory assets under management attributable to clients who are non-United States persons?” Citadel answers that more than $170 billion or 72 percent of its $234.6 billion of gross assets under management are foreign owned…”
*** Senator Warren’s Letter to Ken Griffin ****
Massachusetts Senator Elizabeth Warren addressed Ken Griffin with a scathing letter dated 16 February 2021, stating that (emphasis added):
“…Concerns about this conflict of interest [between Citadel’s ‘payment for order flow’ and its ‘hedge fund side’] became even more salient when, in late January, with no warning or recourse, Robinhood and several other brokerages abruptly changed the rules on its customers, ‘restrict[ing] trading […] in GameStop and other stocks caught in a frenzy’ and raising requirement for ‘how much money an investor using leverage and derivatives must have in their brokerage account after a stock purchase.’ Both Robinhood and Citadel have denied that Citadel had any role in this decision – but Congress and the public deserve clarity on the process of and reasons for these decisions by Robinhood, which had a significant impact on many individual investors.”
***
In September 2021, four months after Citadel Securities contribution to the Gates-Foundation led humanitarian effort to provide India with oxygen gas generators, media outlet Vice reported that court filings suggested collusion between Citadel Securities and Robinhood, thereby protecting billionaire hedge funds while disadvantaging small, retail investors.
https://www.vice.com/en/article/qj87dx/court-filings-spark-citadel-robinhood-gamestop-theories
“Court Filings Spark New Citadel-Robinhood GameStop Theories,” September 29, 2021
“On Monday night, Citadel Securities broke its months-long silence on Twitter to address rumors circulating on social media that chief executive Ken Griffin lied to Congress about his actions leading up to the temporary halting of GameStop trades on Robinhood late January. The GameStop investment craze was largely characterized by retail investors imagining that they are harming hedge funds and short sellers. For months, countless theories and accusations have insisted that Citadel was behind Robinhood’s decision to halt trading on the 28th after other brokerages had halted trading earlier that week. The central thrust of the theory rests on two relationships: that Robinhood received over 35 percent of its revenue last year ($39 million) from Citadel Securities, which pays the app for a feed of its user’s trades before they’re executed, and Citadel helped bail out GameStop short seller Melvin Capital when it started feeling the squeeze.
Robinhood and Citadel have denied this theory, including under oath at Congressional hearings.
The most recent round of rumors trace back to a document filed as part of a class action lawsuit against brokerages including Robinhood and market makers including Citadel Securities, in the United States District Court of the Southern District of Florida on 22 September 2021. The complaint details conversations within Robinhood on January 27th, one of the days trading of Gamestop was halted by various brokerages, as well as conversations between Robinhood and Citadel Securities.
The lawsuit alleges that on January 27, “high level employees of Citadel Securities and Robinhood had numerous communications with each other that indicate that Citadel applied pressure on Robinhood.” Robinhood COO Gretchen Howard allegedly told CEO Vlad Tenev in Slack that she and other Robinhood executives including Jim Swartwout were getting on a call at 5PM with Citadel Securities.
Later that same day, Robinhood Securities President and chief operating officer Jim Swartwout said in an internal chat, "you wouldn't believe the convo we had with Citadel, total mess."
Later that night, the lawsuit alleges that a call was set up between Tenev and a redacted person at Citadel Securities. The lawsuit notes that Swartwout later stated, “I have to say I am beyond disappointed in how this went down. It’s difficult to have a partnership when these kind of things go down this way.”…
***
And so it is that a group of “billionaire philanthropists” - the Bill and Melinda Gates Foundation, PATH, and Citadel Securities decided to help India with their oxygen supply. There is no doubt that the technological advancement which led to the ability to separate oxygen from nitrogen in air brought about by zeolite adsorption can help humanity.
But could it be that this very same technological advancement also demonstrates the means to implement a murder weapon designed to kill vast numbers of people with the goal of enslaving humanity?
***
“Let me tell you the story of Right Hand, Left Hand. It’s a tale of Good and Evil. Hate: It was with this hand [the Left Hand] that Cain iced his brother. Love: These five fingers, they go straight to the Soul of Man. The Right Hand: The Hand of Love. The story of life is this: One Hand is always fighting the other Hand…” Radio Raheem, character from ‘Do the Right Thing’ (first half of ‘Right Hand Love – Left Hand Hate’ message)
*** How to turn a beneficial medical equipment advancement into a murder weapon ***
Let us reconsider the exact same image shown in the figure laid out by Perez-Botella et al. describing the same process – nitrogen adsorption leading to separation of the product, oxygen, from the compressed air entering either Bed 1 or Bed 2 - with just a small alteration. Imagine the two valves at the bottom of each image reversed as shown (with slightly larger dimensions) below. In Bed 1, the air flows in as before and, under pressure the nitrogen is adsorbed by the zeolite. But now the figure shows the valve to the ‘product’ is closed. Consider what would happen if both vales were closed so that the nitrogen is adsorbed, and then the valve to the *vent* rather than the *product* is opened briefly, as shown in the new figure. The remaining gas, made up primarily of oxygen would exit to the atmosphere.
As before, the valve allowing air into Bed 1 would close while the valve allowing air into Bed 2 is opened. At this time, the temperature of Bed 1 would be raised to enable nitrogen desorption while the valve to the product is opened. This would allow *nitrogen* rather than oxygen to be the primary gas constituent flowing into the product tank. While remnant oxygen may also be present, it could be made far lower than the 20% portion which comprises our atmosphere.
The same process could be implemented for Bed 2. Consider that in the left image of this new modified figure, the valve arrangement would lead to nitrogen as the product while oxygen would be vented from Bed 2 in the image on the left.
It is essential to point out that the new technology, the zeollite adsorbent, would be the same regardless of whether the product is oxygen or nitrogen. The mundane technologies of valve timing and temperature control could lead nitrogen to be the actual product of the oxygen generator. Nitrogen is all around us, comprising roughly 80 percent of the air we breathe. But if were substituted for medical-grade oxygen, a patient could die of suffocation in just minutes. By contrast, if oxygen levels were reduced to levels far lower than the atmosphere, patients would suffer over a long period of time in ways analogous to high-altitude sickness.
As the stories of multiple health-care facilities demonstrate, health care workers who are concerned with the many facets of patient care generally just assume that the equipment labeled oxygen supply – actually supplies oxygen.
This provides an opportunity for malevolent actors.
*** An omission in the technical specifications? ***
The document produced by the WHO with the aforementioned acknowledgment of the efforts of the Gates Foundation and PATH appears to lack advocacy for potentially important safety features. The document fails to recommend any requirement that the use of a secondary measurement of oxygen concentration in the tube leading to each patient. The multitude of stories of oxygen deprivation show that this may be important if there is a simultaneous failure of the both the device (via its valve timing) and its oxygen sensor. While the occurrence of such an event through a product via malfunciton might be unlikely, the risk is too high to ignore given that one or more patient’s lives would be at stake. This second measurement should be made by an oxygen sensor made by a different manufacturer from the concentrator itself to improve independence. Ideally, yet a third sensor would be desirable for installation in the line going to the vent to ensure the gas contains nitrogen at levels higher than atmospheric.
Just as important, the additional sensors should be entirely inaccessible by the internet. The authors of the WHO document failed to consider the possibility of a cyber-attack in which the oxygen concentrator (or generator) might be sabotaged by a malevolent actor. In such an instance, a malevolent actor could access the oxygen concentrator (or generator) and simultaneously alter its valve timing and sensor output. Additional off-network sensors would increase resiliency against such a cyber attack.
***
In the spirit of “If you see something, say something,” I will demonstrate, rather than simply describe, what might occur using a fictitious example. This approach is analogous to model of Event 201. A set of events are conjured which might conceivably transpire but which, of course, would not be classified as real-world events. I denote the scenario “Attack 301”.
To set the scene, bad actors are required, but I would prefer not to associate these evil characters with any particular individuals, demography, or culture. Therefore, I will use George Orwell’s book of fiction “1984” to describe the traits of the terrorist group (fictional, of course) in question. The terror organization called the “Inner Party” (in line with Orwell’s classic text) wishes to reset civilization into a global totalitarian dictatorship in which a small group of people control the thoughts and actions of the rest of the population. Their mantra, also laid out in “1984” is that such an aristocratic hierarchy is the natural order of humanity. The fictional Inner Party wishes to subjugate the low and middle population by placing them in a state of permanent surveillance and to eliminate the concepts of freedom and equality among people, and the Inner Party is willing to go to any lengths to achieve this goal.
Our fictitious Inner Party works by infiltrating the existing (nominally democratic) power structure of both the government - including law enforcement and intelligence agencies, the military, and agencies which oversee public health. In our scenario, the Inner Party also controls influential non-governmental organizations and, perhaps most important of all, the entire media. However, at the time of Attack 301, the tendrils of the Inner Party terrorist organization do not fully control the entirety of the government; to achieve the final few steps, the Inner Party recognizes that a catalyst is required.
Their means to attain power (in this fictitious setting) is very simple – they wish to place the population in a permanent state of fear by bringing about a never-ending series of what appear to be pandemics upon the world. Once doing so, the Inner Party intends to implement lockdowns and mandate face-coverings and vaccines to each individual. Both measures are constructed not for the benefit of the population but rather with the goal of increasing the wealth and power of the Inner Party. These measures, in this fictitious setting, do not reduce the spread or severity of the diseases. Instead, they have important outcomes which serve the Inner Party, a few of which are enumerated here:
(1) The measures demonstrate a tangible means of surrendering of freedom ‘for the common good’, expressed under the concept of ‘public health’, and enable the extension of the surveillance state.
(2) They allow Inner Party members to censor those who speak out against the mandates, which limits any other criticism of the Inner Party, once more using the possibility that the health of others would be harmed by misinformation (or disinformation).
(3) The combinations of lockdowns and mass firings of individuals who refuse the mandatory vaccine reduce the economic output of the world, which leads the people to be more reliant on the globally-centralized Inner Party.
(4) The fertility of the world population is reduced by the vaccines (in this fictional setting, of course).
(5) The lockdowns limit social bonding, which also disrupt connections with family and friends.
(6) The (fictitious) vaccines reduce the quality of life through side effects for about ten percent of those who receive it each time a dose is administered. As their health deteriorates, the proletariat increasingly relies on this centralized global group (Inner Party) to provide health care and other services.
The pandemics are themselves based upon real pathogens (perhaps viruses, aerosolized viral clones, or something else entirely) designed to make people sick. For simplicity, I will use the term ‘virus’ to describe them. However, modern science is not capable of producing viruses which naturally spread around the world while maintaining their highly pathogenic properties. This poses a difficulty for our fictitious Inner Party terrorist organization. Their plan to wholly envelope the world with a totalitarian dictatorship necessitates the surrender of freedom due to fear of severe illness and death. And so our fictitious antagonists are faced with a dilemma: they need people to die by some means other than the virus in order to carry out their plan.
In our scenario, the Inner Party would first target the most vulnerable – those who use supplemental oxygen in long-term care facilities. Let’s assume that this Inner Party has provided the care facility with the oxygen generators and/or oxygen concentrators:
1. Separate the most vulnerable fragile patient, after a positive test for the virus, from other patients in a physically different area.
2. Implement a lockdown under the premise that the virus is so deadly and contagious that family members and friends of the sick and vulnerable patients are unable to visit and witness their treatment.
3. Place the patient on oxygen with the gas generator/concentrator functioning properly (i.e., with the gas exiting the oxygen source composed of about 95% oxygen and 5% nitrogen).
4. Use their control of public health apparatus to eliminate decision-making by individual doctors. Instead, utilize the “newness of the disease” to mandate the implementation of treatment protocols which exclude the administration of medicine which might improve the outcome of the patient.
5. Ensure that the required medical protocol include drugs which increase the wealth of Inner Party members.
6. Ensure that the protocol also includes sedatives to the resident to slow breathing under the auspicious goal of ‘relaxing’ an individual who is frightened of the effects of the virus. The protocol might also mandate that a patient be placed on a mechanical ventilator.
Since the virus is ‘new’, health-care workers would be unlikely to challenge a protocol established by a government organization, which is presumably expending all its time and resources researching and advocating for the most effective treatment options.
At this stage, manipulation of the oxygen generator/concentrator with malice is used by the Inner Party to achieve their goals, as follows.
7. After some time- perhaps an hour- passes with the patient having been sedated and placed on oxygen, an Inner Party associate activates the ‘murder switch’ on the oxygen generator/concentrator. It is essential to understand that the ‘murder switch’ need not be activated by a health care worker on site at the hospital or facility. Rather, the ‘murder switch’ might be applied by an associate of our fictitious Inner Party terror organization using an internet connection, as long as the oxygen gas generator or oxygen concentrator can be connected to a network.
The activation of the ‘murder switch’ alters the timing sequence of the four valves at the exit of the two beds as illustrated in the figures above. The ‘murder switch’ also overrides any output from the oxygen sensors which are part of the device. Rather, the sensor output falsified so that that the same value of 95% oxygen appears to be the ‘product’ throughout all time.
Rather than suddenly changing the percent oxygen in the product, one can imagine instead a progressively decreasing percentage. In other words, the percentage of oxygen in the product stream might be ramped down over the period totaling about an hour. The was to accomplish this would be to briefly open the valve venting the tank to atmosphere while the bed is fully charged with oxygen (i.e., with nitrogen adsorbed) at the initial part of a cycle. Meanwhile, for this same short period of time, the valve to the ‘product’ from the tank with the regenerating bed (which contains nitrogen) is left open while its corresponding valve venting to atmosphere is closed. After this short period within a cycle, the valves revert back to their proper settings. The result might be that the gas ‘product’ composition decreases during this step from 95% oxygen down to 85% oxygen (and 15% nitrogen).
After another period of time at this setting (perhaps a few minutes), the delay time for all four valves is slightly increased again, leading to 75% oxygen and 25% nitrogen. In other words, a valve which allows nitrogen to enter the product tank would stay open just a bit longer than before. The increase of delay time for the valves is repeated progressively. Finally, after about an hour, a valve allowing mostly nitrogen into the product tank is open for almost all of the time while the valve venting to the atmosphere is open in order to allow most of the oxygen to escape into the atmosphere. About an hour after the ‘murder switch’ has been activated, the product gas might consist of about 5% oxygen and 95% nitrogen.
8. While breathing oxygen-deficient air, the patient begins to experience symptoms akin to those of high-altitude sickness. According to the Cleveland Clinic (see https://my.clevelandclinic.org/health/diseases/15111-altitude-sickness ) , patients with low oxygen intake due to altitude experience fatigue, shortness of breath, have chest tightness and congestion, experience a headache, and nausea. More severe cases can lead to confusion and fluid build-up in the lungs or brain. Some can experience High Altitude Pulmonary Edema (HAPE). As fluid builds up in the lungs, oxygen cannot be transported around the body, so cyanosis (skin and nails turning blue) can occur. The Cleveland Clinic states some patients experiencing HAPE “feel like they are suffocating” and that they develop a persistent cough. High-altitude cerebral edema (HACE) involves excess fluid on the brain, causing brain swelling. A patient with this condition “experiences confusion, lack of coordination and possibly violent behavior.”
Ultimately, a patient’s heart rate increases as their lungs must work harder to get the limited supply of oxygen into the body, which may lead to a coronary attack. Under extreme high altitude
Because of sedation and the gradual decreasing level of oxygen in our scenario, many patients would not react to a slow progression of symptoms. Those who are capable of reacting rationally may attempt to remove their mask, but they would appear to be in a state of stress and disorientation. The scenario described would pose special difficulty to nurses and doctors because the natural response to someone with these symptoms (turning blue, for instance) is to ensure patient has sufficient oxygen.
A health care worker might assume that the virus has increasingly become more pathogenic and that the patient is acting in an irrational delirium trying to remove the apparent supply of oxygen from his or her face. The worker might respond by pressing the “oxygen mask” (which is actually delivering mostly nitrogen) more tightly against the face of the struggling patient- and also administer more sedative.
However, after the ‘murder switch’ is activated, securing the mask is equivalent to pressing a pillow into the face of the patient. Taken to an extreme, it leads to suffocation. Yet most health-care workers would not know that the oxygen gas concentrator/generator valve timing sequence was compromised, so they would believe they were do all they could to help the patient survive.
If the patient ultimately does die, the death is attributed to the virus rather than the lack of oxygen. And as fear of the seemingly deadly virus increases, our fictitious Inner Party terrorist organization is emboldened to justify additional erosions of freedom through lockdowns and vaccine mandates.
The best part of their sinister plan is that at any time, for example if there were an inspection, the ‘murder switch’ may be deactivated, and the valves downstream of the two zeolite adsorbent beds would revert to normal operation, as depicted by Perez-Botilla et al. Likewise, the oxygen sensors in the oxygen gas generator or oxygen concentrator would be reset to function properly. There would be no trace of evidence that a murder had ever taken place.
(Left – original figure showing functioning oxygen generator, Right – alteration to produce mostly nitrogen.)
If a patient’s vaccination status were stored electronically as ICD code, for example, the precise oxygen concentrator might be used to target and kill that patient. It would be an especially powerful weapon for the Inner Party to use against members of demographic groups known to resist vaccine mandates due to distrust in the government.
Likewise, any individual who led a movement known to voice opposition to lockdowns and mandates could be singled out for murder by the (fictional) Inner Party.
With all the media focused on the evolution of a new species of virus or the development of new and advanced germ-based bioweapons, it may simply be that the weapon of mass destruction was a combination of sedatives (like Midazolam) and a modern version of an individualized gas chamber.
*** “It is as if tens of thousands of my fellow New Yorkers are on a plane at 30,000 feet and the cabin pressure is slowly being let out.” ***
In April 2020, Dr. Cameron Kyle-Sidell, a doctor in New York City, posted a video on Youtube which was professionally recorded by WebMD.
He said the following:
“This is Dr. Cameron Kyle-Sidell, ER and critical care doctor from New York City. Nine days ago, I opened an intensive care unit to care for the sickest Covid-positive patients in this city. In these nine days, I have seen things I have never seen before. In treating these patients, I have witnessed medical phenomena that just don’t make sense in the context of treating a disease that is supposed to be viral pneumonia. Nine days ago, I presumed I was opening an intensive care unit to treat patients with a virus which was causing a pneumonia that was ravaging lungs across the world- starting out as something mild- a cough, a sore throat, and progressively increasing in severity until ultimately ending in something called ‘Acute Respiratory Disease Syndrome –or ARDS . This is the paradigm that every hospital in the country is working under. This is the disease –ARDS- that every hospital is preparing to treat. And this is the disease – ARDS, for which patients in the next 2-6 weeks, 100,000 Americans might be put on a ventilator.
And yet, everything that I have seen over the last 9 days, all the things that don’t make sense, all the patients I see in front of me, all the lungs I am trying to improve – have led me to believe that Covid-19 is NOT this disease and that we are operating under a medical paradigm that is untrue.
In short, I believe we are treating the wrong disease, and I fear that this misguided treatment will lead to a tremendous amount of harm to a great number of people in a very short time. As New York City appears to be about ten days ahead of the rest of the country, I feel compelled to get this information out. Covid-19 lung disease, as far as I can see, is not a pneumonia and should not be treated as one. Rather, it appears as if (it is) some kind of viral-induced disease, most resembling high-altitude sickness. It is as if tens of thousands of my fellow New Yorkers are on a plane at 30,000 feet and the cabin pressure is slowly being let out. These patients are slowly being starved of oxygen. I have seen patients, dependent on oxygen, take off their oxygen and quickly progress to a state of anxiety and emotional distress and eventually get blue in the face. And while they look like patients absolutely on the brink of death, they do not look like patients dying of pneumonia.
I have never been a mountain climber, and I do not know the conditions at base camp below the highest peaks in the world. But I suspect that patients that I am seeing in front of me look most like as if a person was dropped off from the top of Mount Everest without time to acclimate. I don’t know the final answer of this disease, but I am quite sure that a ventilator is not it. That is not to say that we don’t need ventilators. We absolutely need them. They are the only way at this time that we are able to give a little more oxygen to patients who need it. But when we treat people with ARDS, we typically use ventilators to treat what’s called respiratory failure. That is, we use the ventilator to do the work that the patient’s muscles can no longer do because they are too tired to do it. These patients muscles work fine. I fear that if we are using a false paradigm to treat a new disease, then the method (we use to) program the ventilator, one based on the notion of respiratory failure as opposed to oxygen failure- that this method – and there are great many number of methods we can use with the ventilators, but this method being widely adopted at this very moment in every hospital in the country which aims to increase pressure on the lungs in order to open them up, is actually doing more harm than good. And that the pressure we are providing to lungs – we may be providing to lungs that cannot stand it, that cannot take it. And that the ARDS that we are seeing- that the whole world is seeing - may be nothing more that lung injury caused cause by the ventilator.
Now, I don’t know the final answer to this disease. I do sense that we will have to use ventilators. We will have to use a great many number of ventilators, and we need a great many number of ventilators. But I sense that we can use them in a safer way, and (using) a safer method. That safer method challenges long-held, dogmatic beliefs within the medical community and among lung specialists which will not be easy to overcome. But I really believe that they must be overcome. There are hundreds of thousands of lungs in this country at risk, and the time to overcome them is now. I am confident that if those of us who work bedside with these patients, those of us who are witnessing things we have NEVER seen before, despite the many years we have worked and the thousands of patients and diseases we have seen, If we can effectively communicate this to all those who are so important but who are not bedside- the researchers, the administrators, those who procure our resources and make our protocols, the politicians, our own governments - If we are able to convince them that this is different than anything we have ever seen, I am confident that an answer can be found. By that, effective treatments may be discovered. And that a plan to disseminate that treatment can be rapidly deployed. Tens of thousands, and probably hundreds of thousands, of lungs will be protected.
The time for this is now. We are staring into a future in which a great many of our fellow Americans are going to suffer, not to mention people all around the world. For those who will not suffer directly from this disease, from the terrible human cost of this disease, for those who will not lose a family member or a friend -and there will be a great many number of people who will lose somebody close to them. But for those who don’t, they are still going to suffer from the great economic cost of Covid-19. We are all involved in this future, so I urge those of us who are out there, for those who work bedside, I urge you to speak up. We can change this. Thank you for listening. Please spread the message.”
*** Why wasn’t this ‘whistleblower’ video censored while so many others were? ***
With so many would-be whistleblowers censored, why might this message remain on Youtube? Moreover, why would this apparent whistleblower interview be conducted by a professional media organization (note microphone in the video)?
The most effective disinformation campaign combines 99% truth with the most important lie consisting of the remaining 1% being the most important point. I believe the description provided by Dr. Cameron Kyle-Sidell is correct except for the most important point. I suspect he is correct about with his description leading up to and including this one: “These patients are slowly being starved of oxygen.”
However, his very next statement is the one which includes the most important 1% that an Inner-Party-like entity would want communicated to the world, and I suspect it is inaccurate: “I have seen patients, dependent on oxygen, take off their oxygen and quickly progress to a state of anxiety and emotional distress and eventually get blue in the face.” Rather, I believe those the patients were in ‘a state of anxiety and emotional distress’ before the patient removed his or her own oxygen mask.
I will refrain from guessing the possible motivations of Dr. Kyle-Sidell and, in doing so, leave open the possibility that he is a so-called “useful idiot.” The most effective “useful idiot” to a malevolent actor is an expert who makes an honest mistake, yet believes wholeheartedly that he is correct. It would be interesting to know how many times per day, Dr. Kyle-Sidell himself replaced an oxygen mask on the face of a struggling patient who had removed it.
*** Internet connected ventilators exist ***
If it seems far-fetched that a breathing device would be controlled over the internet, consider the following story from https://health.economictimes.indiatimes.com/news/medical-devices/abm-battling-covid-19-with-internet-enabled-ventilators/75367933
April 25, 2020: “ABM Respiratory Care, a Singapore based medical device company focused on the development and commercialization of airway clearance and ventilation solutions, has developed an innovative ventilator which helps healthcare professionals monitor and program the device from anywhere in the world, in real time. ABM is preparing for fast-track approval of its Tele-Ventilator with regulatory agencies in several countries, including India… ABM’s Tele-Ventilator leverages new technology which is 25 times faster and creates 50 times less data traffic than traditional web technologies… ABM’s Tele-Ventilator branded as BiWazeTM ION is based on its BiWazeTM platform developed over the last 30 months and has already US FDA-510(K)-cleared their BiWazeTM Cough system.”
The COVID-19 pandemic has highlighted a shortage of ventilators but also a shortage of trained healthcare professionals to manage the large volume of ventilators when needed. In addition, frequent bedside visits by healthcare professionals to adjust and monitor ventilators increase the possibility of infection thereby pushing an already fragile healthcare system into a further grim situation. ABM’s Tele-Ventilator addresses both issues by enabling healthcare professionals to securely monitor and adjust ventilator settings through their online portal from any location.
***
Approximately six months after the above announcement, the following story was published:
“ABM Respiratory Care adds Peter Soderberg to its Board as Chairman along with raising $10m Series A funding to advance US commercialization plans
October 26, 2020 by Talent4Boards Team
– SINGAPORE, Singapore – ABM Respiratory Care, a medical device company focused on developing novel integrated airway clearance and ventilation solutions, today announced the raise of US$10.3M in Series A funding round led by Advanced MedTech Holdings, a global medical technology leader, and SEEDS Capital, the investment arm of Enterprise Singapore.
The funding will help ABM advance their US commercialization plans.
ABM Respiratory Care also announced the appointment of Peter Soderberg as Chairman of the Board of Directors.
‘We are delighted to have Mr. Soderberg join ABM as chairman of our board of directors,’ said CEO, Vinay Joshi. ’His appointment comes at a great time for the company since we recently completed our Series A funding of US$10.3 million, secured a significant order for our Alpha ventilator, and received 510(k) clearance by the US FDA for our BiWaze™ Airway Clearance System earlier this year. Mr. Soderberg is a seasoned medical industry leader who has decades of experience leading successful medical device companies. ABM Respiratory Care will leverage his experience as we execute our corporate strategy.’
About Peter Soderberg
Mr. Soderberg currently serves as the Chairman of the Board of Directors for Tactile Medical, a publicly-traded medical device company. Mr. Soderberg recently concluded 18 years of service on the board of directors of Integer Holdings Corp., a medical technology company. Mr. Soderberg previously served on the boards of Constellation Brands, Inc. and the Advanced Medical Technology Association. In addition, Mr. Soderberg is currently the Managing Partner of Worthy Venture Resources, LLC, a company focused on growing commercial-stage companies to a global market presence.
Before his semi-retirement in 2010, he served as President and CEO of Hillenbrand Industries and Hill-Rom, and, before that, of Welch Allyn. He has previously held executive positions at Johnson and Johnson in a variety of operations, marketing and management roles, including President of Johnson & Johnson Health Management.
‘I welcome the opportunity to join ABM Respiratory Care as the Chairman of the Board of Directors,” Said Mr. Soderberg. “I’m excited to work with ABM to advance the standard of care in treating chronic and acute respiratory diseases and conditions with their innovative solutions, particularly as they now seek to rapidly establish their U.S. presence.’”
***
As noted by the above article, Peter Soderberg served as Chairman of the Board for Tactile Medical, based in Minneapolis, Minnesota. It turns out that Dr. Mark Melin described a standing relationship with Tactile Medical in a speech delivered in November 2019, as follows:
https://tactilemedical.com/wp-content/uploads/2020/11/M-Mark-Melin-Transcript-November-2019.pdf
Tactile Medical November 2019: “A Physician’s Journey to Understanding Lymphedema and Phlebolymphedema” by Dr. M. Mark Melin, MD FACS RPVI CWSP
Dr. M. Mark Melin:
“Hello, I’m Dr. Mark Melin, I’m a vascular surgeon and we’re going to discuss my personal journey to understanding lymphedema and phlebolymphedema.
Disclosures:
“An Honorarium has been provided by Tactile, I’m a member of the Speakers Bureau for Tactile, and Google images and Tactile images have been utilized for this presentation…”
Dr. Mark Melin serves as an authority on subjects of interest to Tactile Medical because, according to https://www.veindirectory.org/magazine/contributor/mark-melin-md, “Dr. Mark Melin is currently the West Campus Medical Director of the Wound Healing Institute at Mount Health Fairview (University of Minnesota),” a point I will reference again.
Dr. Mark Melin, who discloses payment from Tactile Medical, with Peter Soderberg as Chairman of the Board of Directors, was also named by the periodical Science in an article about the infamous retracted Lancet article in which a company called “Surgisphere,” which falsely portrayed hospitals around the world as having poor outcomes when hydroxychloroquine was used for the treatment of Covid-19. The Science article describes all three of its authors, and Dr. Melin is mentioned in context with Sapan Desai. A large excerpt of the article given for context (emphasis added):
Sapan Desai
Desai had a history of convincing respected researchers of his skill and integrity. One of them, Gilbert Upchurch, department of surgery chair at the University of Florida, wrote last year in a journal commentary that he had only brief encounters with Desai but had nonetheless mentored him remotely and developed an online friendship with him. Upchurch placed the scientist in a group of "amazing and talented young vascular surgeons."
Illinois court records show Desai is facing two medical malpractice lawsuits filed last year. He told The Scientist that he "deems any lawsuit naming him to be unfounded."
Desai has a history of big aspirations and entrepreneurial ventures—some short-lived. His science-fiction blog, corewardfront.com, was meant "to find the most parsimonious route for mankind to establish a meaningful presence in space." In 2009, he wrote that the site would publish fiction "grounded in facts and reality," adding, "the scientific method must be followed … religiously." The blog is no longer published. As a student, Desai won several small National Institutes of Health (NIH) grants for studies of the vestibular system. He started Surgisphere in 2007, when he was a medical resident at Duke University. Surgisphere's initial products were medical guides and textbooks, although Desai has said he was working on big data projects for the company from its birth. In 2010, under the firm's auspices, he founded the Journal of Surgical Radiology—whose editors included researchers with well-established publishing records. It folded in January 2013. Articles from the journal were cited only 29 times in its history, according to Scimago, a journal rating service. Yet an undated Surgisphere web page, no longer accessible online, said the online-only publication had 50,000 subscribers and nearly 1 million page views monthly—which would have placed it in elite company in academic publishing.
Surgisphere appears over time to have shifted its efforts into developing a database of hospital records that could be used for research. When the pandemic erupted, Desai declared that his data set could answer key questions about the efficacy and safety of treatments. Speaking about the finding that hydroxychloroquine increases mortality in COVID-19 patients, the main finding from the now retracted Lancet paper, he told a Turkish TV reporter, “with data like this, do we even need a randomized controlled trial?” Soon after, the World Health Organization temporarily suspended enrolling patients for its COVID-19 trial of the drug.
Immediately after the Lancet and NEJM studies appeared, however, critics identified anomalies in the data. And they doubted that a tiny firm—with a scant public track record in AI, few employees, and no publicly named scientific board—could convince hundreds of unidentified hospitals in dozens of nations to share complex, protected, and legally fraught patient data. Ultimately, despite Desai promising repeatedly to allow an independent audit of Surgisphere, the firm refused to release the raw patient data and agreements with hospitals for an audit, so no one could validate the authenticity of its database.
No hospitals have come forward to acknowledge working with Surgisphere. Indeed, NHS Scotland, which is mentioned as a case study on the company's website, says none of its hospitals worked with Surgisphere and that it would ask the firm to remove an image of a Glasgow hospital from its website.
Science contacted several of Desai's current or former employees or colleagues. Most would not comment. But Fred Rahimi, an Illinois podiatrist and co-author of a paper with Desai, praises the surgeon as highly capable for salvaging limbs, and easy to work with. Through his publicist, Desai cited Mark Melin, a University of Minnesota, Twin Cities, vascular surgeon, as a supporter. Before the retractions, Melin called Desai "a gentleman of the highest integrity" who has "nothing to cover up."
But one physician-scientist who worked closely with Desai several years ago, says, "Just about everyone who knew him would say: ‘I just didn't have a good feeling about him.' … After they'd been with him, most people dissociated themselves from him," the scientist says, declining to be named to avoid personal and institutional embarrassment.
In the decade since completing his medical residency, Desai moved from job to job—at Duke, the University of Texas, Southern Illinois University, and two private Illinois hospitals, according to his LinkedIn profile. "You might say we should have stopped him, which now seems obvious," Desai's former colleague says. "We should have found a way to get together and say, ‘What's going on here?' rather than allowing him to move from place to place. We should have done better as a medical community. We looked the other way."
*** Connections
To recap in reverse order:
1. In May 2020, Dr. Sapan Desai, who co-authored the retracted Surgiphere ‘Lancet-gate’ paper used Dr. Mark Melin as a character reference. Dr. Melin reportedly said that Sapan Desai was “a gentleman of the highest integrity [who has] nothing to cover up.”
2. Dr. Mark Melin disclosed in November 2019 that he received an honorarium with Tactile Medical and also served as a “member of the Speakers Bureau for Tactile [Medical]”.
3. Peter Soderberg served as Chairman of the Board of Directors at Tactile Medical at the same time that Dr. Mark Melin received an honorarium and served as a member of its Speaker’s Bureau. It is reasonable to expect that Dr. Mark Melin interacted with either Peter Soderberg or one of his subordinates in his association with Tactile Medical.
4. Peter Soderberg was announced as the chairman of our board of directors of ABM Respiratory Care, a “medical device company focused on developing novel integrated airway clearance and ventilation solutions” in the message which announced the raising of US $10.3 million in Series A funding for ABM Respiratory Care. Peter Soderberg was a veteran executive in the large pharmaceutical businesses, including a stint as President of Johnson & Johnson Health Management.
5. In this same announcement, the ABM Respiratory Care President touted the fast-track approval of its Tele-Ventilator, said to be capable of “enabling healthcare professionals to securely monitor and adjust ventilator settings through their online portal from any location,” with regulatory agencies in several countries, including India.
6. In the same announcement, Peter Soderberg of ABM Respiratory expressed his excitement in working with ABM Respiratory “to rapidly establish their U.S. presence”.
***
It turns out that Peter Soderberg and his wife run a philanthropic organization. The Elsa & Peter Soderberg Foundation supports “family planning charities” well-aligned with the Bill and Melinda Gates Foundation.
In his book, The Real Anthony Fauci: Bill Gates, Big Pharma, and the Global War on Democracy and Public Health, Robert F. Kennedy Jr. describes in extraordinary detail the exploits of Bill Gates and his outsized influence on the World Health Organization in Chapter 9, titled “The White Man’s Burden” and Chapter 10, “More Harm Than Good.” Three brief excerpts are provided here:
p. 332: “In 2017, the Gates Foundation adopted the goal of administering contraceptives to 214 million women in poor countries. Gates’s contraceptive of choice is the long-term infertility agent Depo-Provera. Population planners have administered Depo-Provera to poor and Black women in the United States since its invention in 1967… Depo-Provera is a powerful poison, with a devastating inventory of wretched side effects… The FDA warns women not to take Depo-Privera for longer than two years, but Gates’s program prescribes at least a four-year course – or indefinitely- for African women and goes to great lengths to avoid warning Black women about the concoction’s many drawbacks…. ”
p. 343-344: “In 2009 and 2012, the Gates Foundation funded tests of experimental HPV vaccines developed by Gates’s partners Glaxo Smith Kline and Merck, on 23,000 girls 11-14 years old in remote provinces of India… Both Merck and Glaxo Smith Kline disclosed in their shareholder report that their profitable performances by their flagship HPV vaccine were top indicators of shareholder value… At least 1,200 of the girls in the Gates’s study – 1 in 20 – suffered severe side effects, including autoimmune and fertility disorders. Seven died. India’s Federal Ministry of Health suspended the trials and appointed an expert parliamentary committee to investigate the scandal. Indian government investigators found that Gates-funded researchers at PATH committee pervasive ethical violations: pressuring village girls into the trial, bullying illiterate parents, and forging consent forms. Gates provided health insurance to his PATH staff but not to any participants in the trials, and refused care to the hundreds of injured girls.”
pp. 330-331: Gates’s fetish for reducing population is a family pedigree. His father, Bill Gates, Sr., was a prominent corporate lawyer and civic leader in Seattle with a lifelong passion for ‘population control.” Gates Sr. sat on the national board of Planned Parenthood, a neo-progressive organization founded in 1916 by the racist eugenicist Margaret Sanger to promote birth control and sterilization and to purge ‘human waste’ and ‘create a race of thoroughbreds.’ Sanger said she hoped to purify the gene pool by ‘eliminating the unfit’ persons with disabilities- preventing such persons from reproducing by surgical sterilization or other means. In 1939, Sanger created and directed the Negro Project, which strategically co-opted Black ministers in leadership role to promote contraception to their congregations… Overpopulation, Gates’s father told Salon in a 2015 interview was ‘an interest he [his son] has had since he was a kid.’ In 1994, the elder Gates formed the William H. Gates Foundation (the family’s first), focused on reproductive and child health in the developing world. Population control was an enduring preoccupation of his son’s philanthropy from its inception.”
***
As for the Soderberg Foundation,
Excerpt, emphasis added: ““While quality health services are lacking around the globe, living conditions in the Los Rieles community [of the Dominican Republic] are especially dire,” says Jessica Millman, Executive Director of the Elsa and Peter Soderberg Foundation…
As part of this new work, Project HOPE will also recruit community health promoters and train them in topics like child vaccination, breastfeeding support, and family planning. A new community health committee, meanwhile, will help identify the greatest needs and promote health education. ‘Improving access to quality health services for women and children is a top funding priority for the Elsa and Peter Soderberg Charitable Foundation,’ Millman says. ‘Embedding sustainability of improvements by working in partnership with appropriate government entities is fundamental in our grant-making. The Soderberg Foundation is excited to provide funding to support clinic improvements knowing that Project HOPE’s relationship with the government will result in long-term sustainable health system improvement.’”
https://powertodecide.org/about-us/funders
“Power to Decide works with some of the most innovative organizations across the country, who share our vision of opportunity for young people and enable us to make it a reality. To join us in giving young people the power to decide if, when, and under what circumstances to get pregnant and have a child, please contact us.”
https://www.chattanoogan.com/2019/9/18/396462/A-step-Ahead-Receives-200000.aspx
Excerpt: “More women in the Chattanooga region will be able to obtain long-term birth control through A Step Ahead Chattanooga, thanks to a grant of $250,000 from The Elsa and Peter Soderberg Charitable Foundation. The news was announced by Soderberg Executive Director Jessica Millman at a major donor event…”
https://www.pathfinder.org/projects/act-with-her
Arguably the best illustration of alignment between the two philanthropic organizations is demonstrated by the charity “Act With Her” which presently cites on its web page only the Bill and Melinda Gates Foundation & the Elsa and Peter Soderberg Foundations as funders for its mission in the countries of Ethiopia and Jordan.
Its stated goal is to “provide girls with support during one of the most crucial life stages, reaching them before or during some of the most common disruptors of their future well-being (such as forced marriage, pregnancy, or school dropout).” [Emphasis added.]
The close proximity of the goals of the Gates Foundation and the Elsa and Peter Soderberg Foundation, when combined with the connections enumerated above, leads to some very pointed questions. Did Bill Gates use links through Peter Soderberg and Dr. Mark Melin (or their associates) to influence Sapan Desai, perhaps by channeling funds to Surgisphere, the company started by Desai? Is Bill Gates the driving force behind the infamous retracted ‘Lancet-gate paper, co-authored by Sapan Desai?
I wish to emphasize the parenthetical “or their associates” for both Soderberg and Melin. Especially in the latter case, someone knowledgeable of the motives of Desai and (if correct) Gates might have attempted to avoid media scrutiny. Nonetheless, it would be useful to know why Dr. Mark Melin advocated for Sapan Desai in his interview with the Science reporter. For example, did anyone suggest to Dr. Melin that it would be appropriate for him to praise Sapan Desai?
*** Attack 301: Assault on Expectant mothers
Consider once more our (fictional) Attack 301. At the outset of our scenario, vulnerable patients are described. The deaths of the most vulnerable patients, who would be older and frail, may evoke less sympathy from the public than the death of a younger person. In order to introduce the most stringent lockdowns and vaccine mandates over a broad group, they also need to evoke such sympathy. A group they might choose would be expectant mothers. They pose a very attractive option to the Inner Party because (1) instinctively, a society protects expectant mothers, (2) they visit the doctor (and hospitals) more frequently, and (3) they would not be as easy to isolate from society as older individuals, which in turn means that other people would be more likely to accept a vaccine.
Let’s suppose that the sabotaged oxygen sources in our scenario remain intact a full year after the first wave of murder. The Inner Party would be able to evoke sympathy with their ultimate goal of implementing a totalitarian regime by now murdering pregnant women instead of older people in hospitals and nursing homes. The Inner Party would focus on unvaccinated pregnant women, and it would be essential for the media to present the families of the victims to demonstrate their regret at having avoided lockdowns and vaccines.
The difficulty faced by the Inner Party is this: Why would a virus harm women a full year after the initiation of a pandemic when it had little effect in the beginning of the same pandemic? One possible answer would be to conjure a ‘new variant’ of the virus. Typically, viruses become more contagious but less deadly over time. There are a few exceptions, and so experts would be required to place a new variant in this exceptional category. The media, fully conrtolled by the Inner Party, would be used to discredit anyone who might initially claim the new variant is not dangerous. Then, once the murders of pregnant women are carried out by restricting their oxygen, the media would be able to ‘verify’ that the discredited source is partially responsible for their deaths. This feeds the model of censorship so important to the Inner Party.
Moreover, our fictitious Inner Party would benefit from severely injuring some pregnant women because these survivors would later give firsthand accounts of their trauma.
*** Foreword for accounts of women diagnosed with Covid-19 while pregnant who survived ***
The following are media accounts from 21 women who were harmed in their pregnancy. All but one survived and attributed their misfortune to Covid-19. The accounts are arranged chronologically by date of their first visit to the hospital. The majority of stories include just one link, but some include two links because different information is provided in each link.
I prefer to show the entire text of the article because I believe it is fairest to the patients, their families, and to the journalists to show the stories with full context available to the reader. This leads to long stories, so I use bold to emphasize the parts of the stories which I deem the most informative and which I would quote if I left out the context.
The women who have been injured want these stories to be read by a wide audience. If even one of these women were hurt intentionally, then she surely deserves compensation from those who harmed her. This article showing all 21 in context may prove to be a beneficial tool.
Please take note of the following: (1) For all but one pregnant woman, ECMO is part of their treatment regimen. (2) The majority of the hospitals where ECMO is used are affiliated with universities. (3) The women remember very little of their experience. (4) Pay close attention to the emphasis on vaccination status and advocacy for stories published after the Covid vaccines were available.
The following link is relevant to the first two stories, which describe incidents which initiated in May 2020, the same month in which George Floyd was also killed. (https://www.epilepsy.com/complications-risks/covid-19/covid-19-and-seizures ).
The Epilepsy Foundation bluntly states that: “Seizures are not a symptom of Covid-19.” It then goes on to note that at end stages of the disease progression of any serious infections, damage to other organs may lead to seizures.
*** Media reports of 21 women diagnosed with Covid-19 while pregnant. ***
1. Aquarius Bunch, Iowa
“I Just Thought I Was In A Dream': One Iowan's Story Of Surviving COVID-19” Iowa Public Radio | By Natalie Krebs , Published July 5, 2020 at 5:00 PM CDT
Though many people who have been seriously ill from COVID-19 are older or have underlying health conditions, it’s still unclear what causes certain people to get really sick from the coronavirus. Waterloo resident Aquarius Bunch had been a healthy 27-year-old working at an assisted living facility when she got COVID-19.
When Bunch tested positive for COVID-19, she quarantined alone at home hoping to ride out her fever and cough.
"I was taking several baths and showers a day. I was checking my temperature. I was drinking tea. I was staying hydrated. I couldn't really eat that much," she said.
But Bunch never got better. Instead, she got sicker to the point where she went to the emergency room in Waterloo.
"I really don't remember much. I just remember they were checking my temperature. They gave me some Tylenol," she said. "And I thought I was getting ready to go home. That's what I remember."
Then Bunch’s condition deteriorated fast. She had a seizure, and doctors decided she would need to be transferred to Iowa City.
"So they quickly contacted our team at the University of Iowa," said Sharon Beth Larson, a doctor at the University of Iowa Hospitals and Clinics, "to say we have a COVID-19 patient who has a periviable fetus. So this is a fetus at an age where it is not likely to survive outside the uterus."
Larson said there was something else to worry about. Not only did Bunch have COVID-19, she was six months pregnant, and her lungs were failing.
"She was at that point, not responsive. She was sedated. She was paralyzed. She was on the mechanical ventilator," Larson said.
Larson, a cardiothoracic surgeon, was called in because Bunch needed more than that ventilator to survive. Her organs still weren’t getting enough oxygen.
Her only chance was a complex, invasive life support procedure known as extracorporeal membrane oxygenation, or ECMO.
Larson said ECMO is used on just 1 to 2 percent of the sickest COVID-19 patients. It involves surgically attaching tubes and monitors to pump oxygen into the blood. This would give Bunch’s lungs a chance to heal.
"And then we can wean the support and let the patient continue to recover," Larson said.
Larson is the surgical director for UIHC's ECMO program. She said the procedure is used on people who have failing hearts or lungs, like those who are awaiting transplants, as type of bridge. This can also work for COVID-19 patients, the odds were stacked against patient like Bunch.
Larson said less than half of COVID-19 patients on ECMO survive.
Plus, there was the issue of Bunch's pregnancy. Larson said patients on ECMO nearly always undergo emergency deliveries.
"There is bleeding complications. There's thrombotic, or blood clot complications. So we were doing the very best we could in this very rare and unique situation," she said.
Larson said during the hour that it took to do the procedure, the room was tense, filled with emotion. A maternal fetal medicine team monitored Bunch’s baby the whole time, ready to deliver if necessary. But it wasn’t. And Bunch made it through.
"I remember waking up and I was on Zoom with my family. They were waving me smiling and, you know, talking to me, and I just thought I was in a dream," Bunch said.
Bunch and her lungs improved rapidly. So much so that a little over a week later, she was taken off of ECMO. The next day her ventilator was removed.
And just two weeks after Bunch arrived in Iowa City by air ambulance, she was sent home to Waterloo to her mother and her 3-year-old son.
"It was actually on Mother's Day I got to come home so that was great. That was amazing. That worked out well," she said.
Bunch said in the whirlwind of what had happened, she never got to talk to Larson while in the ICU. She met her at a check up appointment after leaving the hospital.
"I felt very emotional because, you know, she saved my life. Like I was so glad to be able to see her and express my feelings and emotions about how I felt," she said.
And Larson said Bunch has been a source of inspiration during what she calls a “dark and disturbing” few months at UIHC battling COVID-19.
"Maybe things will never be normal again in the hospital," Larson said. "But it just felt so good that ...we conquered this virus, that Aquarius conquered this virus, that has taken out so many of our friends and family and loved ones and colleagues."
Bunch is now at resting at her home in Waterloo. Her baby girl is due in August.
https://uihc.org/patient-story/ecmo-leads-happy-ending-pregnant-mother-covid-19
ECMO leads to a happy ending for a pregnant mother with COVID-19 , Aug 14, 2020 by UI Health Care
Aquarius Bunch, 27, a pregnant mother who was diagnosed with COVID-19, was discharged from UI Hospitals & Clinics on 10 May 2020 after receiving care from our teams. She spent one week on an advanced form of life support called ECMO, allowing her lungs to rest and heal.
On Aug. 12, Aquarius gave birth to a healthy baby girl named Ka'Oir at our hospital.
She is believed to be the only pregnant COVID-19 patient in the U.S. to have a healthy pregnancy still intact after being on advanced life-support.
2. Takia Morrison, Duke University, NC, 1 October 2020
Great COVID-19 Saves: How ECMO Helped a Pregnant Patient Meet Her Newborn Son
October 1, 2020, By Michelle Antoinette Macalino, Duke Surgery
When a baby is born, one of the first people they meet is their mother. For one newborn earlier this year, this was not the case, for his mother, Takia Morrison, was diagnosed with COVID-19. In the wake of the pandemic, caution and the safety of everyone is crucial, and a team at Duke University Hospital was ready to treat Ms. Morrison.
In the Division of Cardiovascular and Thoracic Surgery, Benjamin Bryner, MD, MS, and Jacob Klapper, MD, took charge in the treatment for this case. Even though COVID-19 is new to the world, their experience with various heart and lung therapies have helped in developing a plan to treat COVID-19–positive patients. In this case, the patient had to undergo extracorporeal membrane oxygenation (ECMO), performed by Dr. Bryner, after further complications because of COVID-19.
Proven Therapy
The patient deteriorated quickly, requiring sedation and delivery of her baby by Caesarean section. She was transferred to Duke while her healthy baby remained with family. At Duke, the ECMO device provided respiratory support in tandem with a ventilator. ECMO is a proven therapy for patients with acute respiratory distress syndrome whether it be from the flu, viral pneumonia, or even COVID-19.
“ECMO is a device that drains blood from the patient’s veins,” says Dr. Bryner. “This drained blood then runs through an artificial lung and finally pumps it back into, in this case, the patient’s vein. This device essentially replaces the work of the lungs.”
At the start of the pandemic there was a lot of uncertainty whether ECMO would be the right treatment for COVID-19–positive patients. To get ahead of the game, Dr. Allan D. Kirk, Department Chair of Surgery, Dr. Joseph Rogers, Chief Medical Officer of Duke University Health System, and Dr. Lisa Pickett, Chief Medical Officer of Duke University Hospital, met with surgeons, the ECMO team, and the medical ICU staff to devise a plan on which treatments would benefit COVID-19–positive patients the most.
“Back in the winter when we knew less about COVID, we spent a lot of time talking with hospital leadership and the intensive care physicians. We’d already considered using ECMO as a viable option, so we started making plans for who we would put on ECMO, and how we would go about doing it safely to protect everybody on the team,” says Dr. Bryner. “This meeting paid off because once the time came, we didn’t have to rush when performing ECMO and the procedure itself went extremely smoothly since we put in hours of preparation beforehand.”
Improved Conditions
Even though ECMO was already considered as a potential treatment early on, the team agreed that using the device would be a last resort. Only a small subset of the population with COVID-19 at Duke University Hospital has undergone ECMO treatment. For this specific case, after the patient’s conditions improved, to further ease her treatment, the team decided to perform a tracheostomy, led by Dr. Klapper.
“Tracheostomy is moving the breathing tube from the mouth to the throat, which allowed the patient to communicate more and perhaps aided in her coming off of ECMO,” says Dr. Klapper. “Tracheostomy is a nice alternative because it allows for the patient to not only communicate more comfortably, but it will also require less sedation.”
By placing the breathing tube in the windpipe, the patient was disconnected from the ventilator, allowing her lungs to gradually start the work of breathing on their own. This recovery stage was also helped with the use of ECMO and it allowed her to recover faster from COVID-19 in general. With the help of the tracheostomy procedure, the patient was removed from ECMO and her tracheostomy tube was removed after making great progress.
Tremendous Teamwork
Fifty days after Morrison's arrival, a celebratory parade of nurses, physicians and others involved in her care gave her a sendoff as she was discharged. She met her son for the first time just outside the doors of Duke University Hospital, where Morrison's mother rushed to hand over her grandson while Morrison was still in her wheelchair.
The success of the ECMO treatment reflects the tremendous teamwork displayed by the surgeons, medical ICU, nurses, staff, and care teams at regional clinics. For COVID-19–positive patients who require ECMO, time is of the essence, especially if they are transferred from local clinics.
“The key factor that allowed us to have positive outcomes with all of our ECMO patients I’ve had so far is that they were referred to us early enough for the patient to be safely transported here at Duke University Hospital,” says Dr. Bryner. “This was very much a successful collaboration between Duke and other local clinics.”
GREENSBORO, N.C. (WGHP) — A little more than a year after she was released from the hospital, Takia Morrison’s health continues to improve.
In May 2020, Morrison went to the hospital at 38 weeks pregnant after falling ill. She tested positive for COVID-19, suffered a seizure, and doctors performed an emergency C-section at Moses Cone Hospital.
She was transferred to Duke Hospital and placed on life support for several weeks.
“It feels like yesterday, I still have nightmares and all kind of things,” she said. “My ICU room at Duke I could hear the helicopter, so I think my room was close to the helicopter pad so a lot of times I can still hear that, I can hear the beeping of the machines, the air sounds that the ventilator makes.”
Morrison was able to meet her son seven weeks after she gave birth.
“I don’t know why I didn’t think we would have the attachment that we have now, because I am his mom,” she said at her Greensboro home.
Happy and healthy, baby Kylan doesn’t stay still long. Like most parents, Morrison said this past year has been tough.
“I have a constant fear of COVID in general, I pull up to the grocery store sometimes and if it’s too many cars I won’t go in,” she said.
Morrison still has some trouble breathing, and said her hospital stay delayed her early education degree. She hasn’t felt safe returning to the classroom.
“It’s scary, and I know everyone’s getting back to how the world was but it’s just still lingering in the back of my mind,” she said.
Right now she remains focused on her children, and her health.
“I look at him like he’s special, because he made it too,” she said, of Kylan.
Morrison is working to get back to Duke in the coming weeks. She explained she wants to say thank you to the doctors and nurses who saved her life.
3. Maria Roque Diaz, Maryland ECMO, gave birth on 28 December 2020 (“got sick on the eve of 19 November 2020”)
Covid almost killed this Latina mom and baby. Vaccinate, she tells pregnant women
María Roque Díaz doesn’t remember giving birth to her second son, Dylan, on Dec. 28, 2020. She had been unconscious and on life support after getting sick with Covid-19 during her pregnancy. But scars on her throat and torso remind her of the ordeal she survived to deliver what she calls her “miracle” baby.
Almost a year later, the Salvadoran mother has one message for pregnant women, particularly other Latinas: Get the Covid-19 shot.”
If the vaccine would’ve been available to me when I was pregnant, I would’ve got it without thinking twice,” Roque Díaz said.
The 27-year-old contracted Covid-19 last year when she was six months pregnant and before Covid vaccines became available.
“I couldn’t breathe. I lived in a second floor, and I felt like I couldn’t go up those stairs,” Roque Díaz said in Spanish. “I told Wilian, my partner, to please take me to the hospital. I couldn’t take it anymore.”
“I was so scared andworried for my baby,” she said.
More than 10 months after the US kicked off its Covid-19 vaccine rollout, only a third of pregnant people nationwide have gotten the vaccines, according to the CDC. Vaccination rates are even lower for Latinas and Black mother, at 25 percent and 16 percent, respectively.
Roque Díaz has since gotten the vaccine, as she’s coped with an arduous recovery and has absorbed the unthinkable – how close she and her son came to not making it. She urges other expectant moms to get vaccinated and avoid putting themselves and their families at risk.
“I may be here with all this additional weight and all these scars,” she told NBC News, “but at least I’m here with my family and kids, enjoying them. But unfortunately, other mothers who had cases similar to mine, are not here with us,” María Roque Díaz, a Maryland Latina, said.
The CDC has reported more than 141,000 confirmed cases of Covid-19 in pregnant people, including more than 24,000 hospitalized and 218 deaths.
Surviving unthinkable risks
When she became sick with Covid-19, Roque Díaz spent a few weeks at a local hospital before being transferred to the University of Maryland Medical Center. She was connected to an extracorporeal life support machine, known as ECMO, since her lungs could not provide enough oxygen to keep her and her unborn baby alive.
The mortality rate of any patient connected to an ECMO machine starts to approach 40 percent, according to Dr. Allison Lankford, an obstetrician and gynecologist who cared for Roque Díaz alongside dozens of other doctors and nurses.
Covid-19 patients like Roque Díaz often require multiple medications and “a great deal of sedation,” Lankford said, to ensure they’re comfortable enough on the ventilator to prevent further injuries to the lungs.
“They’re not aware of their surroundings or what’s happening to them,” the obstetrician said.
In the months Roque Díaz spent connected to the ECMO machine, doctors collaborated with the intensive care unit team to make “decisions for continuing the pregnancy versus the timing of delivery,” Lankford said.
“That is certainly one of the most challenging decisions,” she said. “We’re constantly weighing the potential benefit of delivery for mom versus the risk to the fetus of prematurity.”
Dylan was delivered at 32 weeks by C-section while Roque Díaz was still unconscious. He weighed only 5 pounds.
“I just started to cry”
Roque Díaz was told that she bled more than usual during the delivery, partly because she was on blood thinners to prevent blood clots while connected to the ECMO machine.
Two days after her C-section, her stomach started to swell and doctors found out she had internal bleeding, Roque Díaz said. Though she wasn’t aware of her surgery, she describes her scar, which goes from her chest to just below her waist.
As Roque Díaz remained in and out of consciousness, nurses from the neonatal intensive care unit at the University of Maryland Children’s Hospital who were caring for Dylan would bring him to his mother’s hospital room so he could be close to her.
Roque Díaz missed out on holidays and birthdays as she recovered while unconscious until after Valentine;s Day in February.
“When I first woke up, the first thing I saw was the big scar in my belly. Then I got scared because I realized I couldn’t speak because I was intubated. So I just started to cry,” Roque Díaz. “My heart started racing and I was sedated again.”
When Dylan was healthy enough to be discharged, the teams of health care workers who had cared for him and Roque Díaz celebrated with surprise baby shower.
“It was beautiful” Roque Díaz said. “I realized what was happening after I saw balloons in my hospital room and I saw Wilian.”
Debunking pregnancy and vaccine myths
All of the symptomatically and critically ill pregnant mothers who have been admitted to the intensive care unit at the University of Maryland Medical Center are unvaccinated, according to Lankford.
“Unfortunately, the Latino population is making up a number of patients in the ICU, from the pregnancy side of things, that are unvaccinated,” the doctor said.
The majority of pregnant people remain unvaccinated. A lot of pregnant patients are nervous about taking medication, Lankford said, including getting well-known vaccines including for tetanus and diphtheria.
“Often patients have had a very long journey to getting pregnant and the last thing they want is anything that could potentially jeopardize that,” she said.
“The most important things is just awareness and education,” said Lankford. The Covid-19 vaccine is not only safe, “but the alternative of getting Covid has the potential to bemuch more harmful to both mom and the pregnancy.”
Concerns around fertility have also caused women trying to get pregnant to hold off on getting vaccinated, Lankford said.
“There’s really no influence on fertility,” she said. “It’s actually safer to be vaccinated before pregnancy.”
The CDC “strongly recommends Covid-19 vaccination either before or during pregnancy because the benefits of vaccination for both pregnant persons and their fetus or infant outweigh known or potential risks.”
“We know that in the US alone, maternal mortality has been on the rise. Unfortunately, this pandemic has only contributed to that increase. So, in order to start to make a difference, we strongly encourage everyone to be vaccinated,” Lankford said.
An older toddler who “didn’t know who I was”
Roque Díaz is now back at her Maryland apartment, undergoing physical therapy after being bedridden for months.
She’s also reconnecting with her eldest son, Emanuel, who was 2 when Roque Díaz was hospitalized.
“Now that I’m at home, he calls me, ‘Hey, you,” Roque Díaz said. “That was tough on me because he essentially didn’t know who I was. When he would come near me to carry him, I had to explain to him that I couldn’t. I would tell him to please forgive me.”
Roque Díaz is also slowly trying to go back to work, at least on a part-time basis for now. Her hope is to buy a home and a car as she raises her family.
“I look forward to seeing my children grow up, have health and be with my family,” she said.
4. Jackie Dennis, Michigan (Henry Ford Hospital)
https://www.henryford.com/news/2021/03/covid-double-lung-transplant
DETROIT (March 17, 2021) – Henry Ford Health System performed what is believed to be Michigan’s first double-lung transplant on a Wyandotte woman whose lungs were irreparably damaged by COVID-19 and who two months earlier gave birth for the first time.
Jackie Dennis, 31, a special education teacher at the Huron School District in New Boston, Mich., located about 20 miles west of Detroit, said she is fortunate to be alive and thankful for the care she received at Henry Ford.
“No one expected me to leave the hospital so fast, but I had an amazing team of doctors and nurses,” Dennis said. “After being away so long, I just wanted to get home and be with my family. I missed my husband and baby so much.”
Dennis’ fighting spirit through weeks of adversity made quite the impression on her medical team.
‘We have all marveled at just how amazing and inspirational her progress has been,” said Lisa Allenspach, M.D., Medical Director of Henry Ford’s Lung Transplant Program. “It has been a hard-fought battle on many fronts to get to this day. Jackie’s positive attitude and will to survive combined with the persistence and skill of the surgeons and medical teams – everyone working together, that’s what makes miracles happen.’
Dennis underwent the transplant at Henry Ford Hospital in Detroit on January 16, seven weeks after the birth of her daughter Mia Rose. After one week in inpatient rehab, she returned home on Feb. 19 – culminating a 91-day hospital stay between two hospitals in the Henry Ford Health System.
Ricky Dennis, who along with other family members have been taking care of the couple’s 16-week-old daughter, said he endured some scary and difficult days watching his wife’s health deteriorate.
‘It has been a crazy whirlwind,’ he said, adding that not being able to visit his wife because of hospital visitor restrictions made it even tougher.
Dennis’ medical odyssey began Nov. 20 when her husband drove her to the Emergency Department at Henry Ford Wyandotte Hospital. She was 35 weeks pregnant and had not been feeling well. She had a cough, headache and was having trouble breathing. She had been suffering from preeclampsia, a pregnancy complication characterized by high blood pressure and can cause swelling and in some cases affect breathing.
During the medical evaluation, Dennis received a COVID-19 nasal swab and the test came back positive. She was promptly admitted and one week later, doctors induced her labor at 36 weeks. Mia Rose was born healthy on 27 November 2020, one month before the baby’s expected due date.
Shortly after giving birth, Dennis developed pneumonia and her lung function worsened to the point where she was placed on a ventilator. In many patients with COVID-19, the infection can progress to severe respiratory failure and acute respiratory distress syndrome requiring mechanical ventilation.
On December 10, Dennis was transferred to the intensive care unit at Henry Ford Hospital, a Level 1 trauma center known for its expertise in critical care medicine. She was later moved to the cardiovascular ICU and placed on a specialized breathing machine called ECMO. Henry Ford Hospital is among only a handful of hospitals specially trained and equipped to use this unique type of life-support, which pumps blood from a patient’s body to an oxygenator— an artificial lung located outside the body. It adds oxygen to the blood and removes carbon dioxide replacing the function of the person's own lungs. ECMO is used in critical care situations when a patient is extremely ill and their lungs or heart needs help. Some lung conditions that ECMO may be used for, include care for COVID-19, acute respiratory distress syndrome and other infections. It can be an option when other life support measures have not worked.
‘When things were not looking hopeful, the courage and persistence of the team to go aggressively with ECMO was important in the transition for her to be able to receive a transplant,’ said Hassan Nemeh, M.D., Surgical Director of Thoracic Organ Transplant at Henry Ford.
After attempts to wean Dennis off ECMO were unsuccessful and with no signs her lungs would recover, doctors listed her name on the national organ transplant waiting list in a final attempt to save her life. On January 16, doctors were notified that two lungs were available. Later that day, the transplant was performed by a team led by thoracic surgeon Daizo Tanaka, M.D. and cardiothoracic surgeon Dimitrios Apostolou, M.D.
Dr. Nemeh described the removed lungs as the ‘worst he’s ever seen,’ underscoring the ferocity of the damaged caused by the coronavirus. ‘I really anticipated that Jackie was someone who probably would have been in the hospital for many months as part of her recovery given how sick she was going into the transplant. She has really amazed us all,’ Dr. Allenspach said.
Dennis, who coaches the cheer team at Huron High School, said she constantly reminded herself of the theme the team chose for the school year during her time in the hospital. It was ‘Bring Back the Fight.’”
5. Amy Yamaguchi, CA
Woman Meets Infant Daughter For First Time After Emerging From COVID-19 Related Coma November 18, 2021 / 6:01 PM / KCAL News
(At Cedars Sinai-same hospital as actor, Nick Cordero. The hospitalization happened in December 2020):
“An Orange County woman who became Cedar Sinai's first COVID-19 lung transplant patient awoke after five months in a coma to learn that the surgery gave her the gift of life and of motherhood. Amy Yamaguchi was nine months pregnant when she was intubated as result of contracting the coronavirus. Two days later, doctors performed a C-section, delivering her daughter, who is now 11-month-old daughter.
She was then flown to Cedar Sinai for more advanced care and, ultimately, a double lung transplant.
After five months in a coma, she woke with no memory of being married.
"...and I asked my mom, 'Who is this guy that doesn't leave?' and she was like, 'Amy, that's your husband!' And I was like, 'I'm married?' And she was like, 'How old are you?' and I said, '22.'"
Yamaguchi also didn't remember giving birth. Her daughter was 5-months-old when they met. "It was almost indescribable. There was so much joy after having such a crappy road. It was this beautiful little light that was so fresh," she said of meeting Maren for the first time.
There were, however, serious challenges to get to that moment. Yamaguchi was on an ECMO, a heart and lung bypass machine, for five months. Her husband of two years, Danny Levin, was left to parent their firstborn without her.
"A ton of people helped me out and got me through it because I couldn't do it alone, and I wasn't going to be a single dad," Levin said. "It was scary, but I always knew Amy would be home."
While on the ECMO at Cedars, Yamaguchi's only option for survival became the transplant and she would be the hospital's first COVID-19 patient to undergo the procedure.
"At the time we did it, it was very unclear whether it was the right thing to do. She was running into more complications with ECMO, and we were running out of time," Dr. Michael Nurok said.
The surgery was a success, but Yamaguchi suffered mini-strokes. Though her recovery has been painful at times, she said Maren is her bright spot.
"She makes it worth it. There are days I don't want to get out of bed, but when you put that baby in front of you, I want to reach for her," Yamaguchi said.
While she continues to make improvement, Yamaguchi said her thoughts often turn toward the donor's family.
"There's just so much that had to be taken from a family to give to my family," she said.
That gratitude, said Yamaguchi, is what keeps her from feeling robbed of time and the birth of her daughter.
"Bad things happen to good people and it's not any rhyme or reason to that either. It happened, and I have to move on and let it go, so I can be the mom I want to be."
Since Yamaguchi's procedure, Cedars has done seven more COVID-19 related lung transplants. Her doctors said Yamaguchi has the potential for a long and fulfilling life.
6. Lorena Granados, Stanford, CA
“At 20 weeks along, Lorena contracted COVID-19. She hardly felt sick at first; then a week later she passed out in bed, unable to breathe. Horacio rushed her to the emergency room of their local hospital in San Luis Obispo County, California, where she was admitted and put on a ventilator. Yet she didn’t get better. She got worse.
‘The last thing I remember was hearing the doctors tell me they couldn’t care for me anymore and that I was going by helicopter to Stanford,’ says Lorena. ‘I didn’t remember anything else until a month later when I woke up on ECMO.’…
Doctors at Lucile Packard Children’s Hospital Stanford had a doubly challenging job: keep Lorena alive and keep her pregnant as long as possible. It was an incredibly challenging goal, even for a team that was used to providing the highest level of critical care for mothers and babies.
The first step was getting Lorena on extracorporeal membrane oxygen, or ECMO. It’s a sophisticated heart-lung bypass machine, which oxygenates the blood and then pumps it back into the patient’s body. It acted as Lorena’s lungs because her own lungs had quit working. ECMO is used as a lifesaving device, supporting the patient until the body recovers enough to function on its own. The typical length of time on ECMO is seven to 10 days. Lorena was on ECMO for 45 days.
“If Stanford was not Stanford, this case would have been extraordinarily difficult to manage,” says Yasser El-Sayed, MD, obstetrician in chief. “It took all of us collaborating, sometimes minute by minute, to keep Lorena alive and keep her pregnant so baby Matthias could grow and survive.”
A vast circle of doctors and nurses surrounded mom and baby, each contributing their unique perspective. Meetings between specialty departments—cardiovascular intensive care, critical care, the ECMO team, obstetrics, maternal-fetal medicine, neonatology, and pediatrics—occurred several times a day to discuss Lorena’s condition. Stanford is unique in Northern California for offering two hospitals in one: an adult hospital physically connected to a children’s hospital with experts who are accustomed to walking down the hall and collaborating with one another. From the adult side, Lorena received intensive care for herself, and from the children’s side she received care for her baby. It was the right care in the right moment—just what Lorena and Matthias needed.
“Between the two hospitals, we specialize in both highly complex pregnancies and extraordinarily complicated neonatal conditions, and we’re delivering this care in a profoundly collaborative, coordinated manner. It’s one of our absolutely distinguishing features—something many children’s hospitals do not have—and it empowers us to provide exceptional outcomes,” says Susan Hintz, MD, medical director of the Fetal and Pregnancy Health Program. “Our deeply integrated approach enables us to seamlessly perform a difficult delivery followed by a swift hand-off into the waiting arms of neonatologists and other pediatric specialists who are ready to provide whatever care a newborn baby needs.”
The Johnson Center for Pregnancy and Newborn Services is nationally recognized for its research, best practices, and leadership in its focus area. Lucile Packard Children’s Hospital Stanford is ranked as one of the best hospitals in the nation with Neonatology ranked #3 in the United States, according to the 2021–2022 U.S. News & World Report Best Hospitals rankings.
“Every day, we knew that call might come, summoning our large team of specialists to Lorena’s side to perform a major lifesaving measure,” Yair Blumenfeld, MD says. “You could say we were lucky, but if we were not in an institution that had the highest level of lifesaving technology and a top-quality team of life-support specialists, then luck alone doesn’t help.”
When Lorena was 29 weeks along, her husband got the call that he had to come to the hospital immediately. Lorena began having preterm contractions and the baby was in breech presentation, so a cesarean delivery had to be performed to deliver Matthias.
“They told Horacio that they had to act fast,” Lorena says. “So many hands were working together to keep us alive—it was a miracle.”
Performing a cesarean section while a mother is on ECMO is very different than a standard C-section. It’s rare—so rare that it was the first time in three decades that the Johnson Center’s labor and delivery team delivered a mom while she was attached to ECMO.
“It was a very tenuous situation with a high risk of a poor outcome,” Dr. El-Sayed says. “With ECMO, the patient is put on blood thinners, which makes surgery difficult. Plus, Lorena was still very ill. It took the talents of a large team of clinical adult and child care specialists working together to ensure a happy ending.”
The team had met their goal. They kept Lorena alive on ECMO and delivered a robust premature baby. Matthias entered the world at 29 weeks—young, but not so young that he’d have serious complications. He spent several weeks in the Neonatal Intensive Care Unit (NICU), where he remained COVID-free and received help breathing to support his lungs and help him grow strong.
Despite a successful cesarean section, Lorena was not out of the woods. Within 24 hours from delivery, she started bleeding internally. Trauma specialists, trauma surgeons, and obstetric anesthesiologists were called to perform emergency surgeries over the next few days. Lorena was losing a lot of blood, and her lungs were still very sick. Given the complexity of her case, these challenges were anticipated.
“Luckily, her lungs improved almost immediately once surgery was performed and the bleeding controlled,” Dr. Blumenfeld says.
Lorena remembers feeling depressed when she’d look down at her belly and see all the scars. Plus, she needed constant pain medication. She credits the doctors, nurses, and her family for keeping her going.
“The nurses were so loving and positive. If it were not for them, cheering me on, I’m not sure how I would have continued going,” she says. “I lifted myself up for my kids. My girls know me as a strong woman, and I didn’t want them to see me go downhill and deteriorate.”
After 10 weeks at Packard Children’s, Lorena was released home. Having spent nearly all of February to April 2021 in a hospital bed, she had a lot of recovering to do. She used a wheelchair and then a walker. She needed help doing everything, from toileting to cooking to cleaning. Horacio and her girls, Kaylin (16), Konnie and Kendall (13), stepped up and took over. Today, she’s pretty much back, and her doctors expect a full recovery.
“It made us grow stronger as a family,” Lorena says. “I want people who go through tough medical times like this to know you can make it. Don’t let yourself think you won’t, because you will.”
A month later, Matthias was released from the NICU and joined them. As a preemie he needs extra care, but he’s doing exceptionally well.
“I was struck by Lorena’s incredible strength as she pulled through a severe case of COVID, and what a champ Matthias was as a premature baby,” says Ritu Chitkara, MD.
Lorena treasures her early-morning feedings with Matthias. He stares into her eyes, and they have sweet, private conversations.
“I’m taking in every single moment with him. He’s our last child, and we are so lucky to have him,” Lorena says.
7. April Mager, Kentucky
https://www.lex18.com/news/kentucky-covid-19-survivor-shares-story-of-pregnancy-loss (see also video)
FRANKFORT, Ky. (LEX 18) — As we inch closer to pre-pandemic normalcy, life won't be the same for one central Kentucky mother who was hospitalized with COVID-19.
At 31-years-old April Mager ultimately lost her unborn child during her fight against the coronavirus.
Mager was the first person in her household to test positive for COVID-19.
"I really was one of those people that didn't think I was gonna get it, and then when I did, it just affected me so badly," Mager said.
Her husband and eight-year-old son also got sick but their cases were mild.
Mager developed pneumonia, and on 23 May 2021 she was hospitalized at Frankfort Regional Medical Center. During that visit, Mager also found out she was four weeks pregnant.
"I mean, it was just like, I was so happy I was pregnant."
Mager spent nine days in the hospital. On May 31, she was released with a tank of oxygen to recover at home.
Mager soon found out she lost the baby. Mager says her low oxygen levels ultimately caused the miscarriage.
"I want everybody to know that COVID is real and it has real effects on people. It's still very much out there." She says her family is reeling from the devastating loss, but she wants to share her story to encourage more people to get vaccinated. "It scares me that I'll go to Walmart and I'm just getting over all this and nobody's wearing a mask. Not everybody in there is vaccinated, so I just want people to go get your vaccine if you can."
Mager plans on getting her shot as soon as doctors clear her.
Mager says if she can reach even a few more people with her story and save them from some of the pain and heartache her family is experiencing. It will be worthwhile.
Loved ones of the family have organized a go-fund-me to help pay for the family's bills and groceries.
8. Dakota Vest-Wright, Alabama
https://www.wvtm13.com/article/woman-gives-birth-while-on-a-ventilator-with-covid-19-at-uab/36197222 (with video)
Pregnant woman battling COVID-19 forced to deliver baby early while on life support, Apr 23, 2021
BIRMINGHAM, Ala. —Dakota Lee Vest-Wright, who tested positive for the virus on April 9, was transferred from a Mobile hospital to UAB last week after her symptoms began to worsen. After arriving in Birmingham, Vest-Wright was placed on life support before doctors eventually decided to deliver her baby nearly 11 weeks early in hopes it would relieve some of the stress on her body and help her fight the deadly virus.
According to her husband, Justin Wright, his wife is currently in stable condition but is still receiving help to maintain her oxygen levels. She is also being given blood thinner to address a blood clot found in her leg, said Justin Wright, who has not been able to see his newborn son as he continues to quarantine at home.
Reporter, Brittany: A Covid-19 has a south Alabama woman and her newborn baby fighting for their lives in a Birmingham hospital.
Ian: WVTM 13 News's Chip Scarborough tells us how the virus is keeping one family apart during an all-important time. “This mother and her newborn baby both had to be placed on ventilators at UAB Hospital. Wright tested positive for Covid-19 in Mobile earlier this month and had to be transferred to UAB and had to be transferred to UAB for more critical care. This week, doctors decided to deliver her baby via emergency C-section- 10 weeks early to relieve some of the stress on her body.
(Husband) Justin Wright: “There were other people at her job that had also tested positive, so pretty much 100% sure that’s where she got it.”
Reporter: Justin Wright is not able to be with his wife or newborn child because he’s quarantined in Mobile, also battling Covid. Privacy laws prevent doctors at UAB from discussing the case in detail, but it’s an unfortunate reminder that the pandemic is not over, and another surge is not out of the question.
Unidentified doctor: “ We are really at a tipping point. It could go either way, and it really depends on how we behave now more than any other time.
Reporter: “Since those variants are spread more easily, doctor say, it really reinforces the need for everyone to get vaccinated.”
Unidentified doctor: “Just that little short exposure can cause an infection.”
Reporter: Dakota Wright held off getting vaccinated because she was pregnant. Justin waited because he wasn’t sure he wanted the vaccine.
(Husband) Justin Wright: “But this whole experience with me and her, you know, I would definitely encourage everyone that hasn’t gotten to it to go out and get it.”
Reporter: “This family forced apart by Covid-19, but fighting to be reunited. Reporting in Birmingham.”
Mom recovering from COVID-19 meets newborn son for the first time thanks to UAB nurses, May 12, 2021, Media contact: Hannah Echols
Nurses in the Continuing Care Nursery at the University of Alabama at Birmingham Hospital arranged for an early Mother’s Day gift for their patient — the chance to finally meet her son.
Dakota Vest-Wright, a Mobile resident, was diagnosed with COVID-19 on April 9, 2021, and admitted to the emergency room at a Mobile hospital the following Wednesday. She was transferred to UAB on April 19.
When admitted, Vest-Wright was pregnant with her second child. She gave birth at the UAB’s Women and Infants Center on April 20, the same day she was put on ECMO due to COVID-19 complications. Due to her condition, she was not able to meet her son, Bruce.
ECMO, or extra corporeal membrane oxygenation, is a technology using a portable heart/lung bypass machine originally developed for heart surgery. ECMO takes on the function of the heart and lungs by routing the patient’s blood into the machine, where carbon dioxide is removed and oxygen is added. The blood is then pumped back into the body.
Vest-Wright was finally taken off ECMO on May 6, and the CCN nurses began planning the long-awaited meeting. After almost a month in the hospital, and 17 days after giving birth, Wright finally met her son on May 7, just two days shy of Mother’s Day.
As of May 12, Bruce and Vest-Wright continue to receive care at UAB Hospital. A GoFundMe page has been established to help the family.
9. Amanda Jackson, Minneapolis, MN
Pregnant woman's brush with death shows how COVID-19 risks endure for younger adults:
By Christopher Snowbeck , Star Tribune, May 22, 2021 - 4:56 PM
They talked as if they'd never see each other again.
Darryl Jackson spoke through tears during that video call last month, saying he wished he and his wife could trade places, just before COVID-19 forced her onto a hospital ventilator.
It was a dreaded step for Amanda Jackson, who at 38 was pregnant with the couple's fourth child. As her condition worsened over the days that followed, her husband was stricken with fear.
"I was just waiting for that phone call saying that she had passed," he said.
But a risky treatment of last resort not often used on pregnant women during the pandemic not only helped return Amanda to good health, but kept her on track to deliver her baby in July. Last week, Amanda was back at Hennepin Healthcare in Minneapolis for a checkup that found no lingering problems with her pregnancy.
Doctors say her story shows that they're still learning how best to treat COVID-19 patients. It also is evidence that risks from the pandemic endure even as cases decline and vaccine protection spreads.
"She's a walking miracle," said Dr. Tracy Prosen, a maternal-fetal medicine specialist at Hennepin Healthcare, which runs HCMC hospital in Minneapolis. "We weren't sure if mom was going to make it. We weren't sure if baby was going to make it."
In cases like Jackson's, doctors use technology called extracorporeal membrane oxygenation as a lung bypass machine, redirecting blood outside the body so the lungs have time to heal. But pregnant patients need blood thinners to manage the threat of clotting associated with the technology, called ECMO for short. Those medications can become a risk if doctors need to perform an emergency C-section to rescue the baby.
Some doctors opt for a delivery before using ECMO, but Jackson's baby was just 28 weeks' gestation, meaning she would face significant risks due to prematurity.
"I really applaud the HCMC team," said Dr. Sarah Cross, a maternal-fetal medicine specialist at the University of Minnesota Medical School.
"It’s true, if they had to deliver her while she was on ECMO, it would have been dicey. But the whole thing was dicey. The whole thing was a terrible situation and they had an excellent outcome from it."
Younger patients getting sicker
The Minnesota Department of Health reported 599 new cases of COVID-19 and nine new deaths linked to the pandemic on Saturday. More than 2.83 million Minnesotans have received at least one vaccine dose.
Hospital indicators are improving, but Amanda Jackson's story shows how COVID-19 continues to drive serious illnesses, even in younger adults.
"The whole theme of the last few months, for us anyway, has been younger patients and healthier patients getting very, very sick with COVID," said Dr. Matthew Prekker, a critical care specialist at Hennepin Healthcare.
Even before she learned of the pregnancy in late October, Jackson was vigilant about keeping guard against COVID-19. Yet somehow this spring, the virus came to the family's home in Minneapolis.
She suffered painful headaches and a bad cough and lost her appetite. Going to the emergency room, she felt she wouldn't make it home again. Once admitted, she told her husband: "Don't put me on a ventilator.''
But four days later, doctors said a ventilator was her best hope for recovery.
The last chance was ECMO, which doctors estimate has been used with fewer than 25 pregnant patients sickened by COVID-19. Within a few days, Jackson started showing signs of improvement. After three weeks on the ventilator, she was discharged this month.
Jackson has few clear memories of the hospital stay, but her husband vividly recalls the details.
Their 13-year-old daughter, Persephone, celebrated a birthday in April, and the family had to abandon a beloved tradition — "if we don't all sing 'Happy Birthday' on your birthday, then you're not that age yet," Darryl Jackson explained. As Amanda's condition deteriorated, her husband made certain that their 20-year-old son, Joseph, who attends college in South Dakota, made it home in time to see his mother. An athlete, he tacked a tag from his running bag to the bulletin board in his mom's hospital room.
Earlier in her pregnancy, Jackson opted against immunization for COVID-19 because the vaccines were so new. While she now favors getting a shot, she was troubled by what she felt were inconsistent messages about vaccine safety and effectiveness in pregnant women.
"If I had to tell people, as far as what I think, I would say get vaccinated. Because this stuff is real and it's deadly," she said.
Vaccines and pregnancy
Pregnant women face a dilemma with COVID-19 vaccination, Prosen said, because they weren't included in clinical trials of the vaccines. So there's limited data that's specific to them, although no evidence has emerged of a safety problem.
Not many pregnant women with COVID-19 get as sick as Jackson did, but studies suggest they run a greater risk of serious illness. "COVID is really unpredictable with anybody, but it's even more unpredictable in pregnant people. So, we encourage all of our pregnant patients to consider vaccinations," Prosen said. "I recommend it."
After 31 days in the hospital, Jackson is regaining strength. She's thankful for the support of caregivers, families and friends. And considering how COVID-19 has taken so many, including a friend who died just this month, Jackson feels lucky.
"It's heartbreaking. ... What made me survive, versus her?"
10. Marissa Fuentes, Pennsylvania
“A Pennsylvania woman who spent nearly eight months hospitalized after contracting COVID-19 while pregnant was able to reunite at home with her family in time for the holidays.” 30 Nov 2021
Marissa Fuentes, 29, of Wynnewood, Pennsylvania, was discharged from a rehabilitation facility on Nov. 24, the day before Thanksgiving. She spent the holiday at home with her family, a feat her doctors described as ‘a miracle.’
"Thanksgiving felt very surreal because I was able to sit at the table with my entire family," Fuentes told "Good Morning America." "I wanted to take every single moment in and I didn’t want the day to end because it was so incredible."
Fuentes was around 32 weeks pregnant with her second child in April when she said she started to feel light-headed and short of breath.
Her husband, Adrian Fuentes, took her to a local Main Line Health hospital, where she tested positive for COVID-19 and was immediately admitted and transferred to the intensive care unit (ICU).
Just two days later, doctors did an emergency C-section to deliver the couple's baby, a son named Enzo, who was born nearly two months premature.
Shortly after giving birth, Marissa Fuentes, a teacher, was put on a ventilator and an extracorporeal membrane oxygenation, or ECMO, machine, which removes carbon dioxide from the blood and sends back blood with oxygen to the body, allowing the heart and lungs time to rest and heal.
The mom of two, who was not vaccinated against COVID-19 because the vaccines at the time were not yet fully recommended for pregnant women, spent the next five-and-a-half months on the ECMO machine.
While Marissa Fuentes was sedated and on the ECMO, her son was diagnosed with spinal muscular atrophy (SMA), a genetic disease, not connected to COVID, that affects the nervous systems, according to the Muscular Dystrophy Association.
Adrian Fuentes said he had to navigate making care decisions for both his wife in the ICU and his son in the NICU while he was quarantined at home due to also testing positive for COVID at the same time as his wife.
"I can’t tell you how many phone calls I made every single today to check in on the two of them. Everything was minute by minute, hour by hour," he said. "The ECMO was keeping my wife alive while the SMA was killing my son."
"It was extremely scary. There’s just no other way to put it. It was terrifying," he said.
Enzo was ultimately treated with a one-time IV infusion of a gene-replacement therapy. The newborn spent 54 days in the hospital before he was discharged on June 14, 2021, his original due date, according to Adrian Fuentes.
Enzo would not meet his mom for another three months.
Marissa Fuentes met her son for the first time on Sept. 11, 2021, her 29th birthday and just a few weeks after she first woke up from sedation. The day also marked the first time since her hospitalization in April that she was able to see her 3-year-old daughter, Ellianna, in person.
"Seeing them come through the door was literally everything I could have ever asked for. My eyes filled with tears," she said. "I was able to hold them. It was something that I’ll never forget." Marissa Fuentes used the motivation from that visit to fuel her own recovery, pushing through countless hours of physical and occupational therapy with the goal of going home.
"There were a lot of hard days where I cried thinking nothing would get better," she said. "I had to relearn everything. The first time I sat on the side of the bed it took eight people to sit me up. I had to learn how to stand again. I had to learn how to walk again. I had to learn how to get myself dressed and take care of myself. I had to learn how to talk because I still had the [breathing tube] in."
In early November, Marissa Fuentes was transferred to Bryn Mawr Rehab Hospital, where she set an ambitious goal.
"The first day that I met the doctor at Bryn Mawr I told him, ‘I want to be home for Thanksgiving. That is my goal,'" she recalled. "He kind of looked at me like I was crazy and said, 'That’s only two weeks away.'"
"I told him, 'I do not want to miss these holidays with them,'" she said of her two children. "I was a determined woman."
11. Ashton Reed, Arkansas
Young Couple Urges Others to Get Vaccinated, By Linda Satter, June 29, 2021
Celia Ann Reed was two weeks old when her parents got to hold her for the first time in a hospital room at the University of Arkansas for Medical Sciences (UAMS) Medical Center.
The 3-pound, 6.5-ounce girl was born May 27 in an emergency Cesarean section while her mother, diagnosed with COVID-19, struggled to survive. Ashton Reed, 25, had expected to deliver her first child during the first week of August, after a full-term pregnancy. But she was 30 weeks into her pregnancy – about 10 weeks away from due date – when COVID interfered.
Nine days earlier [18 May 2021], husband Charles Reed, 27, had driven her from their Star City home to a hospital in Pine Bluff when she became dehydrated, which they suspected was connected to her regular bouts of morning sickness.
Instead, she was diagnosed with COVID-19 and sent home to recuperate.
Like a large number of Arkansans in their age group, the Reeds hadn’t been vaccinated against COVID-19. Ashton Reed said she feared the vaccination might hurt her developing child. She said a doctor had told her that the long-term consequences were unknown. Charles Reed said he, too, was wary about possible side effects.
But Ashton Reed acknowledged that even if she hadn’t been pregnant, she probably wouldn’t have gotten the vaccine.
“It wasn’t on my mind. I didn’t take it seriously,” she said.
She worked at the Jefferson County prosecuting attorney’s office as a coordinator of services for elderly crime victims, where she dealt with the public regularly. But she was young and lived in a small town, so she thought she was safe.
The mother-to-be returned to the Pine Bluff hospital on May 21, struggling to breathe, throwing up and unable to stop coughing. She also had diarrhea and a fever.
But there was only so much doctors could do.
On the night of May 26, as her oxygen levels continued to drop to dangerously low levels, she was transferred to UAMS.
At University of Arkansas for Medical Sciences (UAMS), Reed’s oxygen requirements continued to increase and, despite additional oxygen, her pulse ox levels, or the percentage of oxygen saturated in her blood, was dipping down to 70%, much lower than the normal level of 95-100%.
Doctors at first used a nasal cannula, a thin tube, to provide supplemental oxygen to help Reed breathe. Then they switched to a mask that covered her face and was connected to a BiPAP machine, which pushes pressurized air into the lungs, to open them and let in oxygen.
When her pulse ox dropped into the 50% range, doctors called Charles Reed and told him they were planning to induce labor at 11:15 a.m. on May 27, in an effort to save his wife. Data showed delivering could improve her chances of survival.
“Then it got worse, and they said they were going to have to do an emergency C-section,” he recalled, checking the Notes app on his smartphone where he had meticulously recorded his wife’s rapidly changing medical situation.
“At 2:15 p.m., we had our little girl,” the young father said.
Ashton Reed’s oxygen levels shot back up right after the birth. But as relieved as the young father was that both his wife and daughter suddenly had a better chance of survival, he wasn’t able to see either one of them in person.
Then doctors told him that his wife’s condition had worsened. They said a ventilator wasn’t doing enough to help her, and that she needed to be placed on the ECMO machine to keep her alive.
The technology, which became available to UAMS patients in March, removes carbon dioxide from a patient’s blood and sends oxygen-filled blood back into the body. By providing mechanical circulatory and respiratory support, it allows a patient’s heart and lungs to rest.
Meanwhile, the couple’s baby remained in isolation in the Neonatal Intensive Care Unit (NICU), where she was closely monitored around-the-clock for potential health problems.
As the days ticked by and Ashton Reed’s life hung in the balance, Charles Reed felt helpless. He hadn’t seen his wife in person since she was loaded into the ambulance in Pine Bluff for the ride to UAMS, and now he also couldn’t see their baby girl, despite being vaccinated after his wife was admitted to UAMS.
But thanks to Angel Eye cameras on every bed in the NICU that allow parents to watch their newborns through an app on their smartphones, he found some relief.
After six days of being sedated and on the ECMO machine, Ashton Reed was able to fully comprehend that she’d had given birth. The young parents also were able to converse through texts and phone calls, and spent a lot of time accessing the live video of their daughter.
Ashton Reed said she later learned that at one point, “my oxygen was so low I almost had brain damage.”
Finally, on June 10, doctors determined it was safe to let Charles Reed, donned in protective gear, hold his daughter in his arms.
“It was amazing,” he remembered. “I was on cloud nine. When you hold her, nothing else matters.”
The next day, doctors wheeled the tiny girl, wrapped in two blankets inside a clear-covered transport isolette, into the room where her mother had been moved on June 7 after being disconnected from the ECMO machine.
Ashton Reed still had a tracheotomy and a feeding tube. But at long last, her husband was able to be by her side, and she was able to see her baby and hold her for the first time, under the close supervision of four nurses, including two from the NICU and one who specializes in infection prevention.
“It’s probably the most peaceful and completed feeling,” she said. “She completes my life, and Charles’ too. She is such a blessing.”
Nurses snapped the first photo of the happy mom, dad and baby together.
Between coughs indicating she still had some recuperating to do, the young mother said she wanted to get a message out to others who have been reluctant to get vaccinated: “Now I know this is deadly. Get vaccinated.”
Charles Reed agreed.
“I’ve talked to nearly everybody I know lately, urging them to get vaccinated because we don’t want anybody to go through what we went through,” he said. “I almost lost my wife and my child.”
“We recommend vaccination before, during and after pregnancy,” said Nirvana Manning, M.D., chairperson of the Department of Obstetrics and Gynecology in the UAMS College of Medicine, who was on call the night Ashton Reed arrived.
“Millions of pregnant women have now been vaccinated without any significant concerns,” Manning said. “Pregnancy increases your risk of requiring oxygen, being intubated and going to the Intensive Care Unit. We as well as our national societies recommend vaccination of pregnant women.”
UAMS Chancellor Cam Patterson, M.D., MBA, said the hospital is seeing a surge in patients with COVID-19, particularly younger patients, requiring high levels of care, such as being in ICU or on a ventilator.
“It has been heartbreaking for me to see young mothers and fathers in our ICUs requiring mechanical support because of COVID-19 infection,” he said, urging all Arkansans to get vaccinated.
A few days after Ashton Reed was able to hold her daughter for the first time, she was released from the hospital. The new parents said they plan to return to the hospital regularly to visit Celia until she gets bigger and they can take her home, probably about the first week of August.
The couple thanked the UAMS team of specialists who took care of them and their baby.
“It was just a miracle,” Charles Reed said, looking at his wife and daughter. “This is a miracle baby.”
12. Ashley Hernandez, San Antonio, TX
JOINT BASE SAN ANTONIO-FORT SAM HOUSTON, Texas (Jan. 7, 2022) -- A Marine Corps spouse and mother of five was 28 weeks pregnant when she caught a “mild case” of COVID-19 in June 2021.
Ashley Savidge Hernandez felt tired but wasn’t too concerned until she began to have trouble catching her breath. Alarmed for their baby, retired U.S. Marine Corps Gunnery Sgt. Carlos Hernandez drove his wife to Brooke Army Medical Center’s emergency room just to be safe.
Ashley had no idea she and her baby were about to embark on a month-long battle for their survival.
“It all seems surreal to me now,” she said on a phone interview, her voice still raspy from the ventilator. “I had no idea at the time how dire the situation was for me and my baby.”
Rapid Decline
Ashley had received the positive COVID-19 results on a Friday and by Monday, her condition had grown much worse.
“When I went in the room to check on her, I instantly knew something was wrong,” her husband said. “Her breathing was labored, and she could hardly get a full sentence out because she seemed out of breath with each word.”
Hernandez quickly loaded their five young children into the van and rushed Ashley to BAMC.
“I placed her in the wheelchair (and) took her into the ER, but I had to go get the kids and move the van, so I told her, ‘I'll be right back,’” he said. “Those were the last words I said to her, and they haunted me for weeks because at several points I thought God might be calling her home.”
Ashley’s oxygen levels began to quickly dip. Her health care team tried low-flow, then high-flow oxygen, but to no avail. In the intensive care unit, Ashley was told she needed to be intubated, which is when a tube is placed in the throat to help air move in and out of the lungs.
“I remember asking them what that meant, but things got hazy after that,” she said.
Ashley was in and out of consciousness, but vaguely recalls the tubes being removed and the loud hiss of the high-flow oxygen drowning out the concerned voices in the room.
U.S. Air Force Col. Phillip Mason was familiar with Ashley’s case, but thought she was improving until that point – until he got an urgent call.
“Ashley was deteriorating quickly,” said Mason, medical director, BAMC Adult Extracorporeal Membrane Oxygenation Program. “For some people, COVID-19 is a very rapidly progressing disease.”
After consulting with her husband, Mason and his team made the difficult call to put Ashley, now 29-weeks pregnant, on ECMO. “Ashley was on the brink of cardiac arrest without intervention,” Mason said. “We needed to stabilize her to allow for a better delivery and the best outcome for both patient and baby.”
“It was really the last-ditch effort to try and save her life,” Hernandez said. Knowing that felt “like a freight train just smashed into my own chest.”
ECMO Explained
Extracorporeal Membrane Oxygenation, more commonly known as ECMO, is a heart-lung bypass system used when other lifesaving interventions, such as oxygen therapy or a ventilator, have been exhausted. It removes blood from central vessels, oxygenates it, and delivers it back into the bloodstream. In essence, it replaces the natural functions of the heart and lungs while treatments and natural healing of the affected organs take place.
Established in 2012, BAMC has the only adult ECMO center in the Department of Defense and remains one of the few centers in the world with global air transport capability. In July 2013, the ECMO team completed the military’s first trans-Atlantic movement of an adult on external lung support -- a 5,000 mile, nonstop flight from Germany to San Antonio.
“We have a tremendous and unique capability to deploy to a combat zone, initiate ECMO and transport the service member back to a medical center,” Mason said.
While it’s been used for severe cases of influenza and other pulmonary diseases, in more recent years, ECMO has proven lifesaving for some patients with COVID-19-related respiratory failure. COVID-19 patients on ECMO typically have a 50-60 percent survivability rate, Mason noted, which offers an avenue of hope for patients and their families.
“In Ashley’s case, we were running out of options, and were concerned for her baby,” he said. “ECMO was the best course of action for her.”
Ashley’s husband vividly remembers the the call from BAMC, asking for his consent to place her on ECMO.
“I asked if they could wait for one hour so I could get my kids settled with someone, get to the hospital before the procedure, and at least tell her I loved her before she was sedated, but they said there was just no time, they had to move forward, so I agreed,” he said. “I knew what that acknowledgment could mean for her, the baby, and us as a family. It was in God’s hands at that point.”
The Delivery
As a specialized team inserted the ECMO tubes, obstetric and neonatal intensive care unit (NICU) teams were poised to deliver and care for the baby as soon as the team gave the all clear. “Once we got Ashley on ECMO, things began to move very quickly,” Mason recalled.
After the cesarean section, the NICU team rushed the baby to the next room for treatment. Aside from needing a ventilator to aid his 29-week-old lungs, Ashley’s newborn son was otherwise healthy. At the time, the staff didn’t think about the historic nature of the moment, which marked BAMC’s first patient to give birth while on ECMO.
Ashley has no memory of her delivery and the days after were “extremely foggy,” she said. It all “snapped back to reality” when her nurses came in with a poster with her son’s updated height, weight, and hand and foot prints, and she became intent on getting well enough to hold her son.
Due to a 30-day isolation, Ashley was able to see her baby via video chat but didn’t meet him in person until weeks later. “It was heartbreaking,” she said. “I wanted to be with him, to hold him and feed him.”
On July 17, Ashley was finally able to visit with her son in the NICU. Still on ECMO and fighting exhaustion, she sat in a room, donned in a gown and mask, and held her baby for the first time. “He felt very heavy and very small,” she said. “But I was so relieved to hold him.”
Ashley was on ECMO for 30 days, mostly while awake to help build her strength and stamina. But like many ECMO patients, she felt “horrible anxiety” and leaned heavily on her health care team for comfort. She especially relied on her nurses, Roxann Naud and U.S. Army Capt. E.J. Rauch, she said.
“She felt very overwhelmed,” Naud said. “She was very concerned about her baby in the NICU and her other children. We did our best to reassure her and let her know her feelings were very normal and okay; that she will get through this.”
Fortified by seeing her baby, Ashley’s condition began to improve. She was removed from ECMO on July 26 and cleared to return home a few weeks later. “I couldn’t wait to get home to see my husband and children,” she said.
Homecoming
Ashley’s husband drove her home from the hospital. As she slowly walked into her house with an oxygen tank, her normally rambunctious children – ages 7, 6, 4, 3 and 1-- were surprisingly calm. “I sat down and they didn’t leave my side for several days,” she said.
A few weeks later, Ashley and her husband welcomed their new baby, Kyzon, home. Now 5 months old, “he’s doing great – eating and sleeping and laughing,” she said.
About a month ago, Ashley had a checkup and received a clean bill of health. “I’m very grateful that God saw fit that I needed to still be here for some reason,” she said, holding Kyzon tightly on her lap. “I’m also extremely grateful to BAMC for the compassionate care.”
“It was an experience unlike we have ever faced, together or apart, but truly a miracle,” her husband added. “Only by God's grace and both the skill and care of the BAMC staff that my family is whole today.”
While ECMO was key, Mason also credits Ashley’s positive attitude and the hard-working team members who sat by her side, rubbing her temples and feet or brushing her hair when she felt anxious.
“We are absolutely thrilled to see Ashley doing so well,” he said. “It’s been a tough few years filled with heartbreaking loss and amazing survival stories. Ashley’s outcome is energizing for all of us.”
With COVID-19 transmission on the rise, Mason continues to encourage people to get the vaccine. “We have not had a fully vaccinated patient on ECMO or close to being on ECMO at BAMC,” he said. “It’s not too late; please get vaccinated.”
13. Prem Koonkhuntod, Charleston, SC
It was a middle-of-the-night phone call no husband wants to get. “They called me and asked, ‘What do you want us to focus on – your wife or the baby?’”
Terry Koonkhuntod’s pregnant wife, Prem, was on a ventilator at MUSC Health in Charleston, South Carolina, at risk of dying from COVID-19. And she was getting worse, which put their baby in jeopardy, too.
At one point, Prem’s heart stopped beating. To her husband’s relief, it restarted after the intensive care unit team gave her emergency chest compressions and medication.
“I don't ask much from God, but that time, I was just like, ‘Please, God, don't let me be a single dad. I'm not ready,’” Terry said.
How did they get here, he wondered. Just a few days earlier, Prem was home with him and their two kids in Myrtle Beach. She’d been so careful, they thought, taking precautions against the coronavirus. But Prem hadn’t gotten a COVID shot, even as the Delta variant raged across the state.
“She did want to get vaccinated because she wants to be safe. But then again, the vaccine is too new. They haven't done a lot of study on it. So she decided not to do it,” Terry said.
It was a decision they would both come to regret.
On Aug. 3, the day their ordeal began, Prem realized she wasn’t feeling well. “I got sick and coughed. I was worried, so I went to get tested. It was positive. I was pregnant, so I was worried about the baby,” she said in a later interview, her voice still hoarse from the ordeal.
As her symptoms escalated, she was admitted to a local hospital, then transferred to MUSC Health. “The doctor said they have the right equipment over there,” her husband said.
MUSC Health has doctors and nurses experienced in taking care of pregnant women with COVID. Those women are at a higher risk than people who aren’t pregnant of getting severely sick, as Prem now knows. The Charleston hospital also has specialized equipment to help COVID patients, including a type of machine that would become critically important in keeping Prem alive.
“I remember they took me to the room, and the doctor came and talked. After that, they took me to the intensive care unit. After that, I don’t remember,” Prem said.
It was a shocking turn of events for a couple who met years earlier when Prem left her home in Thailand for an exchange program that brought her to South Carolina. She was working in a Thai restaurant in Myrtle Beach when Terry, also born in Thailand, came in for a meal.
They fell in love, and Prem moved to the U.S. They married, had two children and were looking forward to welcoming their third child. Now, COVID was putting everything they’d built as a family at risk.
“The idea that I could lose her came across my mind a lot,” Terry said.
But Prem had something important going for her: a huge team of doctors, nurses, respiratory therapists and other experts working around the clock. “We have had over 100 people involved in her care,” said Daniel Young, M.D., a critical care fellow who was part of that team.
“We’re a big university hospital, and we brought all of our resources to bear. She probably wouldn’t have survived if she weren’t at a place like this.”
Those resources included something Prem wouldn’t have had access to anywhere else in Charleston: ECMO machines. ECMO stands for extra corporeal membrane oxygenation. ECMO coordinator and registered nurse Lucy Linkowski explained what the machine, which is only used as a last resort, can do.
“For patients like this, it pulls blood out of the right side of the heart into a machine, which spins it around and pushes the blood through an oxygenator. That puts in oxygen and removes carbon dioxide. Then, the blood is returned to the patient,” Linkowski said.
“So we return oxygen-rich blood to the patient because their lungs aren’t able to do the oxygenation and the ventilation that they normally do.”
Prem would need every bit of that help. “She had an acute decompensation early one morning. I actually got called when I was on the way in,” said Young, the critical care fellow.
He arrived to find Prem hanging on by a thread. “We made the determination that we needed support beyond what we were able to provide with conventional ventilation. And so we moved really quickly,” Young said.
“I worked with our interventional cardiology colleagues to stabilize her by putting her on ECMO so we could deliver her baby.”
That was a first, said maternal fetal medicine specialist Rebecca Wineland, M.D. “We've never had to deliver a baby while the mother is on ECMO before. At that point, it was life and death for Ms. K.,” she said, referring to Prem.
To everyone’s relief, mother and baby survived. The little boy Prem wouldn’t meet for a few weeks, as the ECMO machine did its work, was tiny, less than five pounds. But Alex’s arrival was a welcome development during an agonizing time for the family.
When Prem finally woke up, she slowly took in her surroundings. “I saw the machine. I felt a little bit scared, but I was happy to be alive. After that, I asked my husband, ‘How’s the baby? What’s going on?’ He didn’t want to worry me too much, but he told me the baby’s strong and healthy. That was good news for me.”
Prem has made remarkable progress since then. She’s working with a physical therapist to recover from COVID’s ravages, and her baby is thriving.
Young is thrilled by their outcome. “To have her and her baby both doing well – that’s the reason we do what we do,” he said.
But his team’s work is far from done. “A lot of the general public doesn't know how hard the staff here in the intensive care units at MUSC and across the state are working. So I think we really need to give a lot of credit to the ICU nurses and respiratory therapists, residents, advanced practice providers and other health care team members who are working really hard around the clock, dealing with this pandemic.”
He encouraged everyone who can to get vaccinated, which greatly reduces their risk of ending up in the hospital.
Wineland said that advice applies even to people who have had COVID. “We're seeing pregnant moms get sick again. Even prior COVID should not be a reason not to be vaccinated now, because the Delta variant is 100% in South Carolina and is continuing to cause devastation to those who are unvaccinated.”
Prem saw that firsthand and doesn’t want other mothers to go through what she and her baby have. “I think everyone, even pregnant women, should take the vaccine.”
Her husband agreed. “If I knew this would happen, I would ask my wife to go ahead and get the vaccine to keep her from getting COVID.”
14. Charma Jonathas, Palm Beach, FL
“Pregnant woman tests positive for COVID-19, gives birth, survives after months on ventilator, ECMO machine, Doctor urges pregnant women to get vaccinated”
“PALM BEACH GARDENS, Fla. — Charma Jonathas has a 4-month-old baby girl, Abagail. Jonathas, whose baby was born in August, is reflecting on the past four months and looking ahead to the future.
"Tested positive and then it all went down from there," she said. "My main goal was to give birth to a healthy baby. The priority was to give birth to her and then take baby. The priority was to give birth to her and then take care of myself after."
Her journey went from testing positive for COVID-19 and then giving birth at a hospital in Martin County. Jonathas was then transferred to Palm Beach Gardens Medical Center for a specialized machine.
"I knew I had to go home to them because, you know, no one does it quite like mom," she said. "That was my main motivation. There was never a time I felt like quitting or giving up."
Dr. Nishant Patel, a cardiac surgeon at Palm Beach Gardens Medical Center, said things progressed quickly. "Tested positive for COVID," he said. "She was relatively stable at that time. Delivered a beautiful, healthy baby girl, and shortly after that had a sudden decline in her lung function."
He said she then went on a ventilator.
"She continued to decline," he said. Staff at the hospital in Martin County then put the call out for an ECMO machine, locating one at Palm Beach Gardens Medical Center. She went on it for months. "It allows her lungs to rest and to heal, and the machine does the work of the lungs," Patel said.
Jonathas said it was a battle to get back with her newborn, three other children and husband.
"Kept pushing every day -- every single day. Every day," she said. "When I woke up, it all came back to me. You know, I felt my belly and I said, 'Wow.' I knew I had had a baby when everything was coming back, and I knew I had to get back to her."
Dr. Leslie Diaz is the infection control director at Palm Beach Gardens Medical Center. "Here is a young lady fighting for her life, fighting to be there for her family," she said. "Her will was enormous to live."
Diaz reflected on this moment with a beloved patient.
"She is an inspiration for me, because the two years of COVID have been very taxing for all of us," she said. "To see her where she is at now, at home with her family enjoying the holidays, is extremely gratifying, and this is precisely the moment where I say, 'I gotta keep on doing it.' It keeps my fuel going to be able to do it for the next person that needs it."
Diaz also took the opportunity to urge pregnant women to get vaccinated for COVID-19.
"You really need to focus and shift your fear in the right stuff, and the fear should be the situation that this patient was in," she explained. "That's fear, the not knowing if you're going to make it home, the not knowing if you are ever going to see your born baby again. … This is a happy ending. This is a very good story, but this is not the common. The common is 85% of patients that would've been in her scenario don't make it."
There was a brief reunion at the hospital between Jonathas and the doctors and nurses who saved her life.
"I felt the love," Jonathas said. "I felt their time and dedication, and I just want to say 'thank you' to the hospital and the staff, the nurses. To make it home for Christmas, I'm truly happy to be home for Christmas."
‘Miracle’ Port St. Lucie woman, diagnosed with COVID while pregnant, recovering from coma
By Lindsey Leake Treasure Coast Newspapers, Published 6:00 AM EDT Mar. 30, 2022
“The oxygen concentrator rumbled softly, permeating the quiet living room. Its clear tubing lay tangled on the tile floor, snaking among toys and winding back along itself, ending in a loop around Charma Jonathas’ ears and in her nose.
She shouldn’t be there, in her Port St. Lucie home on a drizzly January morning, holding her 5-month-old daughter, Abigail. Most people in her position don’t survive.
“I’m a great woman of faith,” she said. “It was by God’s grace that I was able to come this far, to be alive.”
Three months earlier, Charma had been enjoying what she thought was a nap when a gaggle of nurses interrupted her slumber, coaxing her to move her feet.
“I didn’t know they were trying to make sure I was OK and that I was alert,” she said. “They were waking me up from the coma.”
Charma regained consciousness at Palm Beach Gardens Medical Center in mid-October. One of the last things she remembered was giving birth to Abigail on Aug. 19 at Cleveland Clinic Martin North Hospital in Stuart.
She’d never made it home with her newborn.
Being in labor wasn’t the only reason the 35-year-old had had difficulty breathing the day her fourth child was born. As her due date approached, she developed a nagging cough.
Hours before Abigail arrived, Charma was diagnosed with COVID-19.
From baby joy to COVID intensive care
It comes back to Charma in waves, the gravity of the over 100 days she spent between the two hospitals, roughly half of which she was comatose.
“I’m still learning about the experience,” she said. “That was quite some time to be asleep or unaware.”
The induced neuromuscular paralysis shielded her from grasping her proximity to death, to being counted among the over 2,400 Treasure Coast residents who have died from the coronavirus.
Upon diagnosis, her primary concern was a safe delivery. Before long, she was breastfeeding her healthy baby girl — her first after three boys.
Charma’s initial moments with Abigail became more precious than she’d imagined. As her condition deteriorated rapidly, she was transferred to Martin North’s COVID wing. She wouldn’t hold her newborn or any of her other children again until December.
“I just kept on declining. I really didn’t understand the severity of the situation,” she said. “I had no idea home was a long way.”
Charma required supplemental oxygen, then a ventilator. Her lungs continued failing.
A double lung transplant was under consideration, but organs were hard to come by on a good day, let alone during the height of the delta variant’s surge.
She needed an extracorporeal membrane oxygenation (ECMO) machine. Fast.
Defying odds of COVID survival
Two years prior and 30 miles south, Palm Beach Gardens had launched an ECMO initiative.
“It just so happened that once we got the program up and running, we were in the midst of a terrible pandemic,” said Dr. Nishant Patel, a cardiothoracic surgeon at the hospital. “Charma, she was our second patient within a couple of weeks of starting the program.”
The more support a ventilator provides, the more pressure it puts on the lungs, Patel explained. An ECMO machine does the lungs’ work more gently.
Charma was transferred from Martin North on Aug. 31, already “paralyzed with medication,” Patel said. Keeping her deeply sedated afforded doctors greater control over her lung function.
Faith, family drive COVID recovery
Freshly roused from her coma, Charma was comforted by the first words she heard a nurse speak: “[Your] kids are OK.”
Preston, 15; Emmanuel, 3; Joseph, 2; and baby Abigail had been thriving under the care of her husband, Robenson. That was all the fuel she needed.
“I went into fight and faith mode,” she said. “It was difficult, but not for one moment did I ever feel like giving up, because I knew I had to come home.”
Her grit, which she attributed to her New York roots and Jamaican heritage, earned Charma the nickname “Feisty” in the ICU. She was transferred back to Martin North on Nov. 9, free of the ECMO machine but back on the ventilator.
She still had miles to go.
“I didn’t realize that I couldn’t walk until I tried to get up,” she said. “I was like, ‘Oh, wow, I have to learn to walk again.’ ”
Pandemic protocols limited hospital visitors to her mother and husband. But her children’s faces were a cheerful presence outside the window. Church family from Kingdom Reign Ministries in Jensen Beach, where Charma and Robenson are pastors, also voiced their support through the glass.
Charma adopted a mantra: Be home by Christmas. She was taken off the ventilator, but remained hospitalized through Thanksgiving.
On Dec. 2, 105 days after birthing Abigail, her dream came true.
“The moment was surreal,” she said. “The joy of seeing her and all my children was extremely overwhelming.”
Waiting on God’s word to vaccinate
In June, Charma had sensed her medical ordeal on the horizon.
“Spiritually, I knew something was going to take place. I just knew in my heart,” she said. “I felt the need to pray over my family.”
Despite nearly dying, Charma relies on her faith to uphold her decision to remain unvaccinated.
“We’re not interested,” she said Jan. 26, affixed to the oxygen concentrator she still wears nightly. “We haven’t gotten any instruction from God to do it.”
People who are or recently have been pregnant are more likely to contract a severe case of COVID-19, the Centers for Disease Control and Prevention stresses, noting the vaccine is safe for those who are pregnant or breastfeeding.
Immunization is a safe, effective way to prevent severe illness, hospitalization and death, according to the CDC. Everyone 5 and older is eligible for the free vaccine.
Though natural immunity is a byproduct of infection, the extent of protection against future illness varies. Among recovered coronavirus patients, those who remained unvaccinated were twice as likely to be reinfected, a CDC study shows.
Not only could Charma contract the virus again, but she also could transmit it. However, should it be God’s will for her to be immunized, she’s keeping her heart open.
She believes her experience wasn’t for naught.
“I want to inspire,” she said. “I hope that someone who is lying in a hospital bed [will think], ‘Oh my gosh, she survived this? I can too. It’s possible.’ ”
Lindsey Leake is TCPalm’s health, welfare and social justice reporter. She has a master’s in journalism and digital storytelling from American University, a bachelor’s from Princeton and is a science writing graduate student at Johns Hopkins. Follow her on Twitter @NewsyLindsey, Facebook @LindseyMLeake and Instagram @newsylindsey. …email her at lindsey.leake@tcpalm.com.
15. Sarah Mays, Colorado
https://www.uchealth.org/today/pregnant-and-dying-of-covid-how-ecmo-saved-pregnant-woman-with-covid/
Pregnant and dying of COVID-19: ‘Miracle mom’ and baby survive thanks to unprecedented double surgeries
Young COVID-19 survivor pleads with pregnant women to immediately get vaccinated. '“If I would have heard a story like mine, there’s no doubt I would have walked right in and gotten the vaccine."
By: Katie Kerwin McCrimmon, UCHealth
Nov. 8, 2021
The young pregnant woman lay fully sedated and belly down in the hospital intensive care unit, attached to a ventilator that was pumping oxygen into her body at the highest possible settings.
“But COVID-19 had ravaged Sarah Mays’ lungs. Even with the ventilator’s help, her blood saturation levels, which should have been hovering close to 100%, had plummeted into the 70s and 80s. Her vitals were tanking. She was dying. For the surgical team, it was “go time.”
Never during the pandemic had doctors at UCHealth University of Colorado Hospital put a pregnant COVID-19 patient on the last-chance, external lung and oxygenation system known as ECMO, much less delivered a 29-week preemie minutes later.
But the doctors knew that the only way to save Sarah’s life — and the baby girl who wasn’t due for two-and-a-half more months — was to give the mother’s lungs a chance to rest and recover. And that meant racing on the morning of Aug. 18 to gather nearly two dozen medical experts to carefully orchestrate back-to-back surgeries: first connecting Sarah to ECMO, then performing a cesarean delivery.
Sarah’s husband, Andrew Mays, returned to the hospital after a fitful night at a hotel across the street to find that Sarah’s condition had gone “down, down, down” that morning.
No one sugarcoated how precarious things were.
Dr. Tim Tran, an anesthesiologist and cardiothoracic critical care specialist who was overseeing Sarah’s care in the ICU, had to go over the worst-case scenarios. He explained that ECMO (which stands for extracorporeal membrane oxygenation) doesn’t always work for critically ill COVID-19 patients. And, it’s exceedingly rare for doctors in the U.S. and around the world to use ECMO for pregnant COVID-19 patients. The team felt confident that they could save the baby. But no one could promise that Sarah, 32, would survive.
Tran’s warnings devastated Andrew, but confirmed fears that had been gnawing at him.
Especially when he was alone at night, he felt like all of his dreams were crumbling.
“I cried myself to sleep,” he said. “I thought to myself, ‘I’m not getting my wife back. I’m going to be raising a baby by myself.’ Your whole life is over, just like that.”
The couple met when they were juniors in high school back in Michigan. They had been together 16 years and married for four. A year earlier, they bought their dream home, a charming log cabin yards from a river in a beautiful canyon just outside of a town with a perfect name: Loveland. They went fishing, hiking and skiing every chance they got. Their golden retriever puppy, Porter, joined the family a year earlier and, now their daughter would be arriving soon.
Everything seemed perfect. Then everything fell apart.
A COVID-19 infection that Andrew had gotten through work over the summer passed to Sarah in early August when she was just over 6 months pregnant.
Neither Sarah nor Andrew, also 32, had been vaccinated. They hadn’t opposed COVID-19 vaccines but felt like they were getting conflicting advice. Andrew’s mom and sister were begging the couple to get vaccinated. Sarah’s mother opposed the vaccine and her pregnant midwife (who didn’t work for UCHealth) told Sarah she wasn’t getting vaccinated. On top of confusing messages, Sarah hated needles. So, putting off a vaccine seemed like the simplest choice.
When the virus struck them, they struggled with guilt and deep regrets. But, it was too late.
Their family is far from alone.
The clinical trials for COVID-19 vaccines had not included women who knew they were pregnant. Some trial participants became pregnant after enrollment and did well with the vaccines. Still, because there was so little data initially about COVID-19 vaccines for pregnant patients, the Centers for Disease Control and Prevention was slow to release definitive guidance.
Medical experts now know that COVID-19 is extremely dangerous during pregnancy. Only about one-third of pregnant women are vaccinated and health experts have issued urgent warnings pleading with everyone who is pregnant or planning to get pregnant to immediately get COVID-19 vaccines. Month after month this year, the number of pregnant women who have died across the U.S. from COVID-19, has set new dismal records.
Sarah was on the verge of becoming one of these pandemic casualties when a group of highly trained specialists teamed up to give her a lifeline.
The doctors gathered for an urgent Zoom call at about 7:30 a.m. on the 18th.
The surgeries — and the timing of them — would be complex.
Dr. Muhammad Aftab is a cardiothoracic surgeon who led the team that connected Sarah to the ECMO machine.
ECMO is essentially a set of lungs outside of the body attached to a pump. Aftab and his team needed to thread wide, garden hose-sized tubes known as cannula from a vein in Sarah’s neck into her heart. The tubes then pull blood out of the body. The ECMO machine has an oxygenator that removes carbon dioxide from the blood and replenishes it with oxygen. The oxygenated blood then flows back to the heart. Normally, a person’s lungs do this job. For Sarah, the ECMO machine would have to take over.
“Sarah had severe infection and inflammation in her lungs. She had what’s known as acute respiratory distress syndrome (ARDS). The lungs are made of millions of alveoli. Sarah’s were filled with fluid and unable to exchange oxygen,” Aftab said.
“ECMO doesn’t fix that problem. It buys time for recovery and allows the lungs to heal,” Aftab said.
Doctors at University of Colorado Hospital have been doing ECMO surgeries for 10 years and have the largest, most experienced ECMO team in the Rocky Mountain region. Their depth of knowledge and ECMO research have proven invaluable over the last 18 months as critically ill COVID-19 patients needed “Hail Mary” ECMO treatments to survive.
Aftab recently presented research showing that in the early part of the pandemic, from April to October of last year, nearly 63% of COVID-19 patients who went on ECMO survived at multiple facilities. The delta variant hit even harder this year, however, and many unvaccinated patients are arriving at hospitals more gravely ill now, making it even harder for ICU and ECMO experts to save the sickest patients.
ECMO doesn’t work nearly as well for older COVID-19 patients, those who are immunocompromised and those whose organs are already shutting down.
Doctors hoped Sarah’s age and good health before she got COVID-19 might bode well for her; so, they gambled on ECMO.
“We wanted to save two lives,” said Aftab who is also an assistant professor of cardiothoracic surgery at the University of Colorado School of Medicine on the Anschutz Medical Campus.
Little did anyone know that Sarah’s strong heart and a fierce maternal instinct soon would kick in.
Before beginning the unprecedented surgeries, the team of doctors created a detailed, step-by-step plan.
“We had to get the baby out. We were out of other options, but how could we do this safely?” said Dr. Cristina Wood, an obstetrical anesthesiologist, an expert on high-risk pregnancies and an associate professor at the CU School of Medicine.
“We went through everything: ‘OK, we’re rolling the patient in. We’re doing ‘x’ task, then ‘y’ task.’ We went over the plan, line by line, step by step, including contingencies in case anything did not go as scripted,” Wood said.
First, Aftab and his team would connect Sarah to ECMO. Next, obstetric surgeon, maternal-fetal specialist and associate professor, Dr. Camille Hoffman, would take over to do the cesarean delivery. Nurses would then hand off the newborn to a team of neonatal intensive care specialists, who would focus 100% on the infant.
On top of the double surgeries, other logistical challenges loomed. COVID-19 patients breathe better when they are face down or in the prone position. But, in order to do the surgeries, the team needed Sarah on her back. And, to make Sarah’s blood flow well once she was connected to the ECMO machine, she needed an injection of blood thinners. Those same blood thinners posed risks for Hoffman and her team. Excessive bleeding during the cesarean delivery could endanger Sarah and the baby.
The doctors kept thinking — and rethinking — the safest way to proceed.
“It was an amazing effort. I’m so fortunate to work with such dedicated, talented and nationally renowned colleagues. We were able to come together utilizing our sub-specialty training and took turns managing things,” Wood said.
The sheer number of people involved posed yet another challenge. Dressed in full, yellow protective gear with face masks and eye protection to keep them safe from the virus, how would anyone know who was who?
Wood has organized other complex surgeries and simulations of emergency “code blues” in the past.
“Communication is so important. Our faces were covered with masks, goggles and ventilated hoods, so I asked one our nurses to find stickers we could write on to identify each team member and their role,” Wood said.
The nurses found fluorescent pink sticky notes and attached the improvised IDs to everyone’s caps.
Once all of their plans were in place, the team planned to meet hours later at 12:30 p.m. to get started. They booked the largest operating room they could find, one typically used for open-heart surgery.
After the planning session wrapped up, doctors met with Andrew.
Aftab still was dressed in a suit, rather than surgical scrubs. He had been scheduled to see several patients during an outpatient clinic that morning but canceled all of those appointments to focus on Sarah.
As Aftab described how the ECMO machine would work, Andrew wept. He felt responsible for bringing the virus into their home. He and Sarah both kicked themselves when they got sick.
“Whatever you need to do, please save Sarah,” Andrew begged.
Aftab held Andrew’s hand.
“I told him, ‘We are here to help. We are going to take good care of Sarah. We will do our best to give her the best possible chance to survive,’” Aftab said.
Andrew nodded and felt some comfort.
“It made me feel like he was a person too. I was going through serious stuff, but he was going to do everything in his power to save Sarah.”
Before the surgeries started, Andrew had time to visit Sarah once more and give her a pep talk.
He suited up in full protective gear, shuffled into the room and bent far down so he could try to get face to face — or in this case, mask to ventilator — with Sarah.
Her eyes were closed.
“She was completely out of it,” Andrew recalled.
Still, he prayed that somehow, she could hear him and feel his love.
She had been riding what doctors described as the “COVID-19 roller coaster” for weeks. People who are sick with the coronavirus — both at home and in hospitals — can seem to improve, then get worse, then rebound again and suddenly crash. That’s one of the reasons why COVID-19 is so dangerous.
And, it’s partly why Sarah got so sick. She thought she was recovering. Then, she couldn’t breathe.
COVID-19 had hit both Andrew and Sarah hard in early August. He had attended a small in-person meeting at work. One co-worker was vaccinated and didn’t get sick. The rest soon tested positive. Andrew tried to keep his distance from Sarah, but two days after he got sick, so did she.
At one point, Andrew got dehydrated and both he and Sarah went to the ER at UCHealth Medical Center of the Rockies in Loveland. Sarah was coughing, but staff members took their vitals, said they were OK and sent them home to recover.
Over time, Andrew started to improve and Sarah hoped she was a day or two from feeling better too. Instead, she declined dramatically. She was coughing around the clock and couldn’t catch her breath. The woman who loved zigzagging up hiking trails soon could not stand up in the shower or climb a single flight of stairs to the couple’s master bedroom.
Sarah’s grandmother in Michigan was so worried one day that she sent an ambulance to bring Sarah from her home in the Big Thompson Canyon back to the hospital in Loveland. The paramedics called when they were en route. Sarah thought she could tough it out and told the paramedics they didn’t need to come.
Finally, after about two weeks of struggling, Sarah knew it was time to get help. Andrew took her to an urgent care facility. Her oxygen saturation was low: 84%. The providers called an ambulance, which took Sarah first to the hospital in Loveland, then on to University of Colorado Hospital, where specialists could better care for Sarah and her baby.
She arrived on Aug. 13 and had to go on a ventilator the next day.
Now, after five days and multiple ups and downs, she was heading into surgery. Andrew was terrified but tried to be positive for Sarah.
“I was quite emotional,” Andrew said. “I held her hand and stroked her leg. I tried to be calm so I could calm her down. I told her everything was going to be fine. She needed to be strong.
“Sarah is not good with doctors, hospitals, needles and all of that. It was very, very stressful before she got put on the vent. But you feel like there’s a glimmer in there.
“I was trying to convince both of us that everything’s going to be OK.”
He promised Sarah that soon they would both meet their baby girl.
“I can’t wait to get both of you home,” he said.
Then, Andrew had to say goodbye.
Soon after Andrew left Sarah’s room, doctors got a new, ominous update.
“Sarah had worsened. Everyone was worried that her heart was going to stop. If a pregnant woman codes, neither she nor her baby are going to live unless we act quickly,” said Hoffman, the obstetric surgeon.
“We were hoping for a little more time,” added Wood, the obstetric anesthesiologist. “But, we obtained additional labs and realized we had to pull the trigger. We needed to go.”
The doctors raced into the operating room ahead of schedule and got underway by about 10 a.m.
As planned, Aftab began. He and his surgical fellow, Dr. Jeremy Leonard, connected Sarah to the ECMO machine. The procedure took about an hour and went very well. Immediately, Sarah began to rebound. Her vitals were looking good and her oxygen saturation levels climbed back up close to where they belonged.
In fact, Sarah looked so good so quickly that Hoffman wondered for a moment if she should delay the cesarean delivery and give the baby more time in her mom’s belly.
But the team persuaded Hoffman that it was best to proceed as planned. The ECMO machine was doing its job, but sustaining another life is hard work and Sarah needed a break. “The physiology of pregnancy takes a lot of blood flow from the mom and sends it to the placenta for the fetus. If the mom is dying, you want to let all the blood return to the mom. You take the baby out as a life-saving measure,” Hoffman said.
At 11:42 a.m., tiny Kabrini Mays made her debut. She weighed 3 pounds, 4.9 ounces and stretched 15 inches long.
“She looked great for a 29-weeker,” Hoffman said. “She was vigorous. She was pink. She made a little crying effort, which is always heartwarming.”
Kabrini was named after the Mother Cabrini Shrine along I-70 west of Denver. On ski trips, Sarah and Andrew always noticed the sign and thought the name spelled with a “k” would be perfect for a girl.
Hoffman handed the newborn off to neonatal expert, Dr. Jim Barry, and his team from the NICU.
By about 1 p.m., the surgeons were finishing up and both mother and baby were doing remarkably well.
The doctors were in awe of what they had just experienced.
“I’ve never been through anything like this. I will never forget this case,” Hoffman said. “We came together quickly. Everyone interacted so well as a team.
“The best-laid plans worked out as well as we possibly could have hoped. There were so many steps and everything went exactly as planned. That never happens in obstetrics. We all were so happy and relieved,” Hoffman said.
Most ECMO patients need to stay on the machine for 10 days to 2 weeks, some even longer.
Sarah proved to be anything but typical.
After just three days, Sarah was becoming more alert and felt a desperate pull to meet Kabrini and reunite with Andrew.
“She woke up on the 21st and said, ‘I’m going to be out of here in two days,’” Andrew recalled.
A day later, Sarah got to see her daughter via video.
“That motivated me to get out of bed,” Sarah said.
Andrew cuddled with Kabrini and told her, “Mommy loves you and is going to see you very soon.”
Sarah was rebounding far faster than anyone expected.
It wasn’t really a surprise to Sarah.
All along she had had a feeling that she was going to survive. She remembered almost nothing from the time she arrived at the hospital. And, she had a sense of how rough things had been on Andrew.
“I know how terrified I would have been. But, all along, I kept hearing his voice. I heard, ‘You’re going to be fine.’ He must have been saying those things to me,” Sarah said.
As Sarah improved, the ECMO team decided to test Sarah’s lungs. They clamped the cannula on the ECMO machine — without removing them — to see if Sarah could maintain her oxygen levels.
She did well.
Her next challenge was to regain some strength.
In order to do that, her team needed her to get up and try walking.
The blood-filled tubes from the ECMO machine still were attached to Sarah’s face and neck and felt extraordinarily heavy.
“Three or four nurses were helping me stand up. I could barely walk to the chair, but I was determined,” Sarah said.
Along with working on her physical strength, Sarah started pumping her breastmilk for Kabrini.
“I wanted her to have the antibodies,” Sarah said.
Wood, Sarah’s obstetric anesthesiologist, credits Sarah’s maternal instincts for her speedy progress.
“Moms are the strongest people in the world. Sarah was so determined. She walked around with these huge bypass tubes. The strength it took her to overcome that, to get off ECMO and go see her baby was incredible. I work with a variety of patient populations, but mothers always impress me the most,” Wood said.
On Aug. 22, Andrew and Sarah learned that Kabrini was having trouble with her bowels.
She had malformed intestines that had developed early in the pregnancy and had nothing to do with Sarah’s case of COVID-19 or Kabrini’s premature birth. Kabrini would need to receive care next door at Children’s Hospital Colorado.
The next morning, Sarah learned that Kabrini was about to be moved. She enlisted a nurse to rush her in a wheelchair to the NICU for a quick visit before Kabrini’s transfer.
“I need to go see my baby,” Sarah told her nurse.
While it’s complicated to detach ICU patients from all of their monitors, Sarah’s nurse sprang into action.
“She ran me as fast as she could,” Sarah said.
She sped Sarah in a wheelchair down two floors in an elevator then far across the hospital to the NICU.
“I got to hold Kabrini for two hours. It felt like 10 minutes,” Sarah said. “I gave her lots of hugs and kisses. I told her I was going to see her very soon and that she was going to be just fine.
“That gave me even more motivation to get better.”
By Aug. 23, Sarah’s team removed the ECMO tubes and by Aug. 26, she got to leave the hospital, far sooner than anyone had expected.
“We were absolutely flabbergasted that she was getting out so early,” Andrew said.
Kabrini ended up needing surgery to fix her malformed intestines. She stayed at Children’s for several weeks and Sarah and Andrew visited every single day. For the team at Children’s, Sarah was a celebrity of sorts. Everyone took to calling her the “Miracle mom.”
Kabrini, too, seemed motivated to bust out of the hospital early. Her doctors expected her to need to stay at Children’s close to her original due date at the end of October. Instead, she was released on Oct. 8 and got to spend Halloween at home, where Kabrini donned a mermaid costume.
“Everyone at Children’s was so sweet and luckily Children’s is the No. 1 pediatric gastrointestinal hospital in the nation,” Sarah said.
These days, Andrew and Sarah feel blessed to celebrate every milestone, including their recent wedding anniversary.
Andrew can’t stop kissing his “girls.” After all his family endured, he is relishing simple moments.
Kabrini is growing fast. She now weighs 8 pounds, more than double her birth weight, and she is nearly 20 inches long. She loves to make funny faces and expresses herself with her arms.
Both Andrew and Sarah — and all of their doctors — are on a mission to encourage people to get their COVID-19 vaccines. They want all people, including those who are pregnant, to protect themselves and avoid scary ordeals, like the one the Mays endured.
“If I would have heard a story like mine, there’s no doubt in my mind that I would have walked right in and gotten the vaccine right away,” Sarah said. “I strongly encourage everyone — particularly pregnant women or those who want to get pregnant — to get the vaccine.
“If I had gotten vaccinated and still got sick, chances are I could have fought the virus more easily,” Sarah said. “Please strongly consider it. I went back and forth so much and I wanted to do the right thing.”
Andrew already has received his first two vaccine doses. Sarah’s doctors recommended that she wait 90 days after being released from the hospital. She’s now slated to get her first vaccine dose around Thanksgiving, an occasion when her entire family will mark the holiday with extraordinary gratitude.
Dr. Tran, Sarah’s ICU doctor, also is pleading with people to get vaccinated.
“It’s remarkable that Sarah survived,” said Tran, who is an assistant professor at the CU School of Medicine. “Sarah was very fortunate. A lot of people aren’t as lucky.”
Nearly all of the people who are dying now of COVID-19 are unvaccinated. Their illnesses are largely preventable, Tran said.
Sarah’s survival gave caregivers a big boost just when they needed it.
“We are all very demoralized,” Tran said. “Please get vaccinated.”
Both Sarah and Andrew have some post-traumatic stress from all that they endured. While Sarah was released from the hospital quickly, she temporarily lost her speech and suffered deficits in her short-term memory. She has fully recovered now, but still has crazy flashbacks and dreams, which is typical for people who have been sedated in ICUs for long periods of time.
“I dream that I’m roaming the hospital. I’m acting like a nurse and going into patient rooms. That’s funny because I’ve always been terrified of blood and needles. But, I always wanted to go into the medical field,” Sarah said.
Sarah helps manage programs that provide before and after school care for children in northern Colorado. She’s back at work now, as is Andrew, who works as a general foreman for a telecommunications company.
Andrew never will forget the day when he finally knew everything was going to be OK.
Kabrini was still at Children’s Hospital Colorado but was doing well.
Andrew and Sarah needed to check on their house and their dog. Their neighbors kindly had jumped in to help as the couple spent their days at the hospital with Kabrini and nights in Aurora at the Ronald McDonald House, a charity that provided them a free home away from home.
Smoke from wildfires had blocked views of the mountains for weeks over the summer and into September.
As the couple turned west from I-25 toward Loveland, Longs Peak and Mount Meeker, two beautiful, soaring peaks, jutted up into crystal blue skies.
“It was one of those moments. I couldn’t say a lot. But, it hit me. I was driving and I had my wife beside me,” he said. “It was the first clear day.”
They drove farther, and as always, felt immediately at home in their canyon, with its stunning beauty and a churning river that has carved a path through soaring walls of granite. They got closer to their home, crossed one bridge over the Big Thompson and another over a smaller tributary.
There, they found their neighbors lined up in their front yard.
“They welcomed us home,” Sarah said.
She and Andrew teared up over the simple, kind gesture.
“You start to appreciate everything and not care about the little things,” Sarah said. “I look at life differently now. I’ve always appreciated my life. But, without all the help I got, I wouldn’t be here watching Kabrini grow.”
Andrew, too, often feels utterly in awe of his miraculous wife and baby.
“There are no words to describe how grateful we are. If it weren’t for Sarah’s nurses, doctors, surgeons and prayers from around the world, we wouldn’t be here.”
Back at the hospital, during the scariest days, Andrew’s mom flew in from Michigan to support her son. She’s Jewish and brought Andrew a special “hand of God” bracelet to help ward off evil and protect his wife and baby.
“Do not take it off until Sarah and your baby are home,” Andrew’s mother told him.
Andrew wore the bracelet around the clock. And when Sarah’s survivial was most in doubt, Andrew held his wrist to his wife’s hand, pressing the omen to her skin and hoping to pass along the bracelet’s healing powers.
“It’s a beacon for people who need help,” Andrew said. “I felt an extremely strong need to keep it on and to know that I had it with me.”
The bracelet seemed to work.
“I felt prayers coming to me. It was the strangest feeling,” Andrew said.
Sarah and Kabrini did indeed make it home. And once mother and baby were safely out of harm’s way, Sarah and Andrew joined hands and slid the bracelet from his wrist to hers.
“We always have it on to help protect our family,” Sarah said.
The couple plans to raise Kabrini in the Jewish faith, and when she celebrates her transition to adulthood, Andrew and Sarah plan to give her a very special gift.
“At her Bat Mitzvah, we will give her the bracelet.”
16. Katie Pederson, CA
https://abc7.com/pregnant-covid-baby-woman/11028786/
Expectant mother, on life support at UCLA Medical Center, survives COVID with her pregnancy intact By Denise Dador
Sunday, September 19, 2021
SEAL BEACH, Calif. (KABC) -- A pregnant Seal Beach woman survived a harrowing COVID infection after UCLA doctors took extraordinary measures to save her life and the life of her unborn baby.
In an interview with ABC7, Katie Pederson explained why she waited to get vaccinated and what she wants other expectant moms to know.
When Pederson found out she was having a baby, very few pregnant women were getting COVID-19 vaccines.
"I was going to wait until my third trimester until it was more readily available and there was more information. I felt safe in my decision -- until I wasn't," said Pederson.
Twenty-four weeks into her pregnancy, she tested positive for COVID. Her symptoms were getting progressively worse when she went to seek care at an Orange County emergency room.
"They admitted me, and that's the last time I saw my husband for about three and half weeks. I was intubated and put under. That's when I thought I was going to die," Pederson said.
"Once the breathing tube went in, it became pretty clear that her lungs weren't going to sustain her," said Dr. Peyman Benharash with UCLA Health.
He and his mobile ECMO team transported Pederson to Westwood. To provide oxygen for her and her baby, the team inserted cannulas into her arteries.
"That removes blood from the patient and, in this particular case, adds blood and removes carbon dioxide and then returns the blood to the patient," Benharash said.
Doctors said she's one of many pregnant COVID patients to need life support. During pregnancy, a woman's immune system is suppressed so as to not attack her fetus. This makes a pregnant individual highly susceptible to severe illness.
"For the majority of patients, they end up having to be delivered while still on the ECMO machine," said Dr. Christina Han, an OB-GYN specialist.
She said Pederson was one of the rare circumstances where doctors were able to take her off the heart-lung machine.
"I remember every nurse and doctor say 'You're awake? How? And you're still pregnant?'" Pederson said.
She's now 35 weeks pregnant with a baby boy. But Pederson is still recovering from the mental and physical fallout of being in the ICU. She doesn't want any other pregnant woman to wait like she did to get vaccinated.
"What's right for me is protecting my body and getting vaccinated," Pederson said.
“For the majority of patients, they end up having to be delivered while still on the ECMO machine," said Dr. Christina Han, an OB-GYN specialist. She said Pederson was one of the rare circumstances where doctors were able to take her off the heart-lung machine.
"I remember every nurse and doctor say 'You're awake? How? And you're still pregnant?'" Pederson said.
"We now know that these vaccines are not raising any red flags at all. There is no risk of stillbirths, of miscarriages or of preterm delivery," said Han.
When Pederson's son is old enough, she said, she wants to tell him: "We fought this. You are super strong. And we did it."
17. Kristina Wiltse, Washington (state)
This pregnant mom nearly died from Covid. It hasn’t convinced her to get the vaccine, Oct 05, 2021
The Covid vaccines are safe and effective during pregnancy. And yet, two out of three pregnant people are unvaccinated.
Having Covid during pregnancy is far more dangerous than if you weren’t pregnant. Covid puts birthing people at risk of being hospitalized, ending up on a ventilator, and having to deliver preterm.
And yet, fear of the unknown has kept two-thirds of pregnant people from getting the vaccine.
Kristina Wiltse, 31, is one of them. Wiltse lives with her partner and three kids in a trailer about 20 minutes from Shelton, on an island with no cell service. She said she doesn’t trust the Covid vaccine.
“I've had so many bad experience[s] with vaccines that have been fully tested,” she said. “This vaccine — I feel like it's even a higher risk than other vaccines.”
She doesn’t believe it’s been tested enough, or that we know the long-term effects.
In August, Wiltse was 28 weeks pregnant with her fourth child when she started getting a cough and a sore throat. It was Covid.
After a few days, “I couldn’t get up and walk to the bathroom without losing my breath,” she said.
She decided to go to the hospital. She wanted to protect her baby.
“I could feel her moving around and everything, but even with movement, you can’t tell what the heartbeat is,” Wiltse said. “I couldn’t get air. I figured if I can’t get oxygen, then she’s not getting it.”
Wiltse drove to the nearest hospital and collapsed into a wheelchair. They spent the night trying to help her, but they couldn’t, so they airlifted her to the UW hospital in Montlake.
That helicopter ride in the bright morning light is the last thing Wiltse remembers until she woke up five days later.
“My hand immediately went down to my stomach, and I realized the baby wasn’t there,” she said. “And I pressed the call button on my bed and I had a nurse come in.”
The nurse had to suit up in full PPE before coming into the room.
“I pointed to my stomach,” Wiltse said. And the nurse asked, “Are you in pain?”
Wiltse couldn’t talk because she was intubated, and on an ECMO machine — a heart and lung machine that pumps blood out of the body, oxygenates it, and pumps it back in.
“And I shook my head no and I motioned for a pen, and he got me a whiteboard and a dry erase pen,” Wiltse said. “And I wrote down, ‘Where’s my baby?’”
The nurse told her that her daughter was in the newborn ICU and doing well.
Wiltse’s worries had come true: Neither she nor her baby had been getting enough oxygen. The doctors had to perform an emergency C-section, even though it was nearly three months before the baby’s due date. Wiltse’s daughter was born severely underweight — only two pounds, six ounces — and couldn’t breathe or eat without help from machines.
Tanya Sorensen, a maternal-fetal physician at Swedish Hospital in Seattle, said her worst fears are unfolding.
“We're seeing many, many more pregnant women getting infected and severely infected and in the ICU, and dying and having premature babies,” she said. “It feels a little desperate.”
In August, more pregnant people died of Covid in the U.S. than any other month since the beginning of the pandemic.
In late September, the Centers for Disease Control and Prevention released a health advisory once again urging pregnant people to get vaccinated.
Pregnant Asian-Americans have the highest vaccination rate, at 47 percent. Pregnant Black people have the lowest, at 17 percent.
Srilata Remala, founder and co-director of the Maternal Coalition, said there’s a lot of confusion. Her organization advocates for equitable and safe maternal health, with a focus on people of color.
Remala said some people are confused about which is more dangerous: Covid, or the Covid vaccine.
“I think they’re misunderstanding some of the stories of pregnant people dying of Covid versus of the vaccine,” she said.
She said she hopes that all the safety data and consistent messaging about how the vaccine protects the pregnant person, their baby, and their community can start to change perceptions.
Megan Felling, a midwife in Olympia, said getting her patients to accept the Covid vaccine has been a struggle. She tells them that data shows the vaccine is safe and effective during pregnancy, and that they can share their immunity with their baby, who will then be born with some protection against Covid.
“There are some of my clients who won’t — for whom that’s not compelling, for whom there’s just a real lack of trust in pharmaceuticals,” Felling said. She said some of them have “a real fear that, oh, we’re going to find out years down the line that actually it wasn’t safe, and I will have made a choice to do something that put my baby at risk.”
Kristina Wiltse said, if she had it to do over, she still wouldn’t get the vaccine.
“I’d rather go through that, because I was able to make it through that,” she said. "I don’t know that I’d be able to survive the vaccine just because of how my body reacts.”
Wiltse spent almost a week on an ECMO machine. Hardly anyone survives that, but she did. And, after a week or so on a ventilator, she was able to breathe on her own again.
Finally, Wiltse was disconnected from enough machines that nurses could wheel her through the hospital to go see her baby.
“I felt like she was just this little porcelain doll that I was gonna break because she was only two pounds six ounces,” she said.
“I told her everything about her brothers and her sister and her dad,” she said. She told her she’d be okay and that “she's my little miracle baby, and I was never gonna leave her again.”
A few weeks later, Wiltse was discharged from the hospital. The ICU nurses in the hallway applauded as she left.
“Nobody there knew if I was going to survive,” she said. “Nobody knew if my baby was going to survive.”
Wiltse drives the two hours to Seattle every few days to see her baby and drop off breast milk she’s pumped for her.
Her own recovery has been rough: Doctors have had to reopen her C-section scar twice to deal with infections and fluid. The hole in her throat where the ventilator tube entered her trachea is healing slowly, and she’s starting to get her strength back while fighting off postpartum depression.
Her daughter Aurora weighs more than three pounds now. Wiltse hopes to bring her home around her due date, in mid-November.
18. Diana Crouch, TX
After nearly dying of COVID-19, a Texas mom encourages pregnant women to get vaccinated
KERA | By Eleanor Klibanoff | The Texas Tribune
Published February 8, 2022
The COVID vaccine is proven safe during all stages of pregnancy, and pregnant patients are at an increased risk of getting seriously ill if they contract the virus. Still, many pregnant women hesitate.
When Diana Crouch found out she was pregnant, she started taking every precaution she could to keep herself and her baby safe. She exercised often, drank water and tried to eat right. She even stopped using her usual facial cleanser because she was worried about the chemicals.
So when her doctor talked to her about getting vaccinated for COVID, she balked.
“I just didn’t want to risk it,” she said. “I was like, we have an immune system for this, and I don’t want to do anything that might affect my baby.” In April 2021, when Diana got pregnant, less than 20% of pregnant people nationwide were vaccinated for COVID. Now, more than 65% of pregnant people are vaccinated, but OB-GYNs say they’re still battling significant fear and misinformation.
Time and again, they say, patients tell them the chance of complications from the vaccine is too high, and the chance of getting seriously ill from COVID is low.
But that is a complete inversion of reality.
“We have so much data that [the vaccine] has been shown to be safe in all three trimesters of pregnancy,” said Manisha Gandhi, chief of maternal fetal medicine at Texas Children’s Pavilion for Women and Baylor College of Medicine. “And then we have continued evidence that having COVID when you’re pregnant and unvaccinated definitely has worse outcomes for both mom and the pregnancy.”
Pregnant patients are more likely to get seriously ill from COVID, and getting COVID while pregnant increases the chances of giving birth prematurely or losing the pregnancy altogether, according to the CDC. And while the vaccine has been proven to be safe, there’s far less data when it comes to the safety and efficacy of COVID treatments for pregnant women.
“If your thought was, hey, I don’t want to get a vaccine because I don’t want to introduce something into my pregnancy, you’ll be introducing a lot of other things when we have to start treating you for a complicated COVID-19 infection,” said Gandhi.
That’s what Diana found out the hard way when she showed up at the hospital with a headache and fever in her second trimester. She wouldn’t leave the hospital again for nearly five months — and, even her doctors agree, it’s a miracle she left at all.
The worst-case scenario
When Diana got pregnant, she and her husband Chris were thrilled to be adding another child to their growing blended family. Chris works as a deputy with the Harris County Sheriff’s Office, and Diana took care of the four kids they shared, including a now 2-year-old born just a month before the pandemic hit.
Diana’s pregnancy was totally normal. In fact, when she was in her second trimester, she felt well enough to travel so she and Chris went to Las Vegas for their anniversary. When they returned, she had a really bad headache, which her doctors initially chalked up to dehydration.
But then she developed a fever and her oxygen levels started dropping. At the hospital in their suburb north of Houston, they diagnosed her with COVID pneumonia and transferred her to Texas Children’s Pavilion for Women. By the time she got there, she couldn’t breathe.
“The last thing I remember was them telling me that they were going to put me on the ventilator,” she said.
Texas Children’s is a level IV maternal care facility and throughout the pandemic, the staff has cared for a lot of pregnant women battling COVID. The best, and most common, scenario is to deliver the baby before the patient needs to be put on a ventilator or extracorporeal membrane oxygenation (ECMO).
“We’ve had a bunch of 30-, 31-weekers where the baby was delivered prematurely to lift that extra strain for mom,” said Cameron Dezfulian, director of the Adult Congenital Heart Disease ICU at Texas Children’s. “In some of those cases, after the delivery is done, they get so much better by not having that space filled with the baby.”
But Diana was only 18 weeks along. A fetus cannot survive outside the womb before a minimum of 24 weeks of pregnancy. They couldn’t deliver — they were going to have to treat them together.
Doctors put her on a ventilator, but two weeks later, she wasn’t improving. That’s when they started talking to Chris about putting her on ECMO, a last-resort life support machine that would serve as Diana’s lungs outside of her body.
“I did research on that, and it was just bad,” Chris said. “It’s a coin toss if you’re going to live once you get on ECMO, and some of the doctors said it’s less than that.”
There have been only a handful of cases of pregnant patients being put on ECMO to treat COVID, particularly this early in the pregnancy, Dezfulian said.
Diana was sedated, so Chris had to navigate this impossible situation by himself, balancing his wife’s prognosis against the viability of their child, while confronting the very real possibility that neither could be saved.
“I may go home without anything,” he said he remembers thinking. “With a dead baby and a dead wife … there were some really dark days.”
He agreed to put Diana on ECMO, which Dezfulian thought was the best chance to save both mother and baby. And it seemed to be working. She started to improve, enough to come out of sedation, and they got her to 25 weeks of pregnancy, past the point at which the fetus could potentially survive outside the womb.
That was what they’d all been working toward, and yet, even that came with significant complications.
“Once that baby was viable, then all of a sudden, we had to plan for at any moment we might have to deliver him,” Dezfulian said.
They set up the room next door as an obstetrics operating room and had doctors and nurses on stand-by, prepared to deliver, while still hoping to get more time.
“The outcomes get better with every week,” said Dezfulian. “As long as we didn’t think the baby was causing harm to her, we wanted to get them both through as long as possible. She had voiced that from the start, that she wanted to give her baby the best chance possible.”
A turn for the worse
Nearly two months after Diana was admitted, Chris and Dezfulian thought she and the baby had turned a corner. But then, she suddenly had three strokes and a heart attack, while Chris and her father watched.
“Being pregnant, having COVID and being on ECMO are the three major risk factors for blood clots,” Dezfulian said. “COVID also puts you at risk for bleeding. She’d had significant internal bleeding for weeks,” which limited their ability to use blood thinners.
Diana ended up in a coma, and the doctors were back to working without a playbook. Dezfulian met with Chris, took his hand, and they prayed.
“It’s the first time I’ve ever had a doctor pray with me and I didn’t know how to think about that,” Chris said. “Because when a doctor is praying with you, you know there’s not much else … we can do.”
Chris said the doctors told him that they’d see how she was doing in the next seven days.
“I was like, ‘Well, what happens in seven days?’” he remembers asking. “And they just said, ‘We’ll cross that bridge when we get there.’ So that’s when I knew she has to get better this week.”
On the fourth day, Chris took her hand and asked her to give him some sign that she was still there and still fighting. He squeezed her hand. She squeezed back.
“That’s when I knew we were going to get out of there,” he said.
Dezfulian still remembers that moment, and Chris’ certainty that the situation was going to turn around.
“I just felt this sense of reassurance,” Dezfulian said. “Seeing him feel that way and knowing that was coming from his prayers. That made me feel a lot more confident that we were doing the right things.”
Diana continued to improve, and finally, at 31 weeks of pregnancy, she delivered a healthy baby boy by cesarean section. They named him Cameron, after Dezfulian.
“My first response was, I don’t deserve this,” he said. “This was such a team effort. No one physician, nurse or anything can take more than 0.1% credit for this.”
Encouraging others to get vaccinated
In all, Diana spent nearly five months in the hospital, including 51 days on ECMO. She was in and out of sedation and doesn’t remember much about this period, including delivering Cameron.
She didn’t even know she’d given birth until three days after it happened, when a nurse from the neonatal intensive care unit brought him up to visit.
“I was still kind of in and out, so it was kind of blurry for me. … It was really hard to not be in my right mind,” she said. “It was really emotional.”
Cameron was released from the NICU after a month, but Diana stayed in the hospital for several more weeks. She was finally released on Dec. 23, just in time to spend Christmas with her children, who had been looked after by her parents during her five-month hospital stay.
She left the hospital on oxygen, with a chest tube to prevent her lungs from collapsing. She can’t really hold Cameron, because she still doesn’t have full strength in her left arm from the stroke. She’s doing physical therapy five days a week.
And she’s still dealing with the emotional toll of her experience.
“When you’re out of it for so long, you just wake up and [find out] all these things happened to you,” she said. “Every time [Chris] retells the story, there’s something new, like something I hadn’t known before.”
Five days after she was released from the hospital, Diana received her COVID vaccine. She wants other pregnant women to learn from her experience.
“After all I went through, the least of your worries should be the vaccine,” she said. “I put my baby through all this as well.”
Chris got vaccinated, too, when Diana was in the hospital. He’s conservative, and he said when he raises it with his unvaccinated friends and family, he sometimes gets pushback.
“But I’m not getting into politics with them,” he said. “I just say, if you can eliminate what happened to me, if you can do damage control, why not do it? Why risk it like we did?”
19. Misty Monson, Indiana
'He’s my miracle baby': Brownsburg mother shares COVID-19 journey during pregnancy
By: Nikki DeMentri , Posted at 11:05 PM, Jan 20, 2022
BROWNSBURG — Simply put, COVID-19 during pregnancy changed Misty Monson’s life.
Before contracting the virus, Monson said her family took precautions, but also lived their lives. Monson said her husband David was in and out of grocery stores for work during the height of the pandemic and the family stayed safe. “I kind of thought of it like a cold, like the flu. I didn’t worry about it too much,” Misty Monson said.
Chase was the final piece of the puzzle for the Monson family. Misty said she knew her third pregnancy would be her last and in the early months, it went smoothly.
“Everything was good. I felt great. There was no indication that anything was wrong,” Monson said.
That all changed at 29 weeks. Monson said, like normal, she was running around town with her children to different practices and school when she noticed she could not taste. She got a test and quarantined until she got the results – it was positive.
Monson’s husband tested positive as well; her two children did not.
After quarantine for several days, Monson was advised to go the ER where she was soon transferred to Ascension St. Vincent. What happened next was a blur.
“To be all alone it’s a little scary — even as an adult,” Monson said.
“While hospitalized, her condition quickly worsened, and she was moved to the ICU. “I just remember screaming and just asking them to help me breathe. I couldn’t breathe,” Monson said. Nine days after first being admitted, she was placed on both a ventilator and ECMO.
“One person started putting in a port and another person was putting in one ... and I just sat there and I was like please slow down just a little bit so I can see my husband," Monson said. "I didn't know if I was gonna wake up afterwards or be the same or be me when I do, and so like I just want to tell my husband that I love them."
During the week she remained on life saving machines, Monson gave birth via emergency C-section, nine weeks before her due date. Her little boy was named Chase. He weighed just over three pounds and went straight to the NICU.
“It’s an experience I hope I never have to do again,” Monson said.
Almost a week after he was born and after Monson was removed from ECMO and a ventilator, the now mother of three was able to meet Chase for the first time.
Monson was discharged in late September 2021, but went back religiously until Chase was released right before Thanksgiving.
“It becomes very emotional between the provider and the patient and I just remember her looking at me and saying you know please do everything you can to keep me alive so that I get to meet my baby,” Dr. Tovah Buikema, the Director of Maternal Fetal Medicine at Ascension St. Vincent, said. She led Monson’s care team.
Dr. Buikema said pregnancy and COVID-19 is ever changing with each wave.
“We’re seeing a much higher risk of stillbirth and much higher risk of devastating outcomes for the fetuses and the babies, very devastating effects on the moms and pregnancies,” Dr. Buikema said.
At the beginning of this month, the CDC estimated around 40% of pregnant Americans ages 18-49 were fully vaccinated. Dr. Buikema, along with other public health experts, urge vaccinations among pregnant and breastfeeding women.
“I think that those of us that are taking care of these patients are just begging our patients that have been hospitalized to go back to their communities, and help us spread the word of what can happen to otherwise healthy patients who contract COVID-19 during pregnancy,” Dr. Buikema said. “I think that we feel like we're doing the best job that we can as the OB providers in the community, but sometimes, it has to come from the patients that have survived the worst of the worst. We’ve asked Misty and all of our other patients that have been lucky enough to survive the worst case scenario to go back to their communities and help us advocate to the pregnant moms in their community to get the vaccine and to do everything they can to try and avoid being the next statistic in the ICU.”
Monson was not vaccinated when she went through her journey. At the time she got pregnant, Monson said there was not much information out there when it came to vaccinations and pregnancy. In the days before she got the virus, her and her husband were doing more research on it after she had a discussion with her doctor.
“I did just go get my shot because I never want to put my family through that again. It was a scary, scary three months," she said.
Today, Chase is gaining weight, smiling and learning tummy time. Monson is just grateful to be here, to continue being a daughter, a wife and a mom. She thanks her and Chase’s care teams for their unwavering support both in and out of the hospital.
20. Lareesia Wight, Phoenix, AZ
PHOENIX - A Phoenix man lost his fiancée to COVID-19 complications on Christmas Day after a hard-fought battle with the virus that lasted more than three months - and he does not want her to be just another statistic for COVID-19 deaths.
Despite this tragedy, a healthy baby boy was born who will never know his mother. Maurice Turner is still trying to process the grief.
"I just want to let people know to take it serious," Turner said.
On Christmas morning, he lost his fiancée, 30-year-old Lareesia Wright. Turner says they both caught COVID-19 in late August, despite taking the pandemic seriously.
"We just wore our masks all the time, and we really didn't go anywhere," Turner said.
Wright was a mother of two and pregnant with a boy approaching the due date. Coronavirus caused her to have breathing issues, and she went to the hospital, Turner said.
Her son, Maurice III, was born premature. Wright would begin ECMO treatment at Banner University in September 2021 and fight for her life for the next three months.
"She did everything she could to try to come home, but it's hard, man," said Turner.
He was never able to hear his fiancée's voice since then, raising the three children they shared together on his own.
He admits they hesitated to get vaccinated during the pregnancy, and now Turner has received his shot.
"I hate that she had to go through this for it to really open up my eyes, but I knew what I had to do," he said.
According to the CDC, there are nearly 40,000 women with COVID-19 who completed their pregnancy. Almost 20,000 were infected during the third trimester, like Wright.
Turner wishes she was still here, but will remind their baby boy how much she loved him.
"I would honestly trade my life for her," he said.
Visit the family's GoFundMe here: https://www.gofundme.com/f/support-for-weedie-b-wright-family-expenses-fund
21. Cierra Chubb, Lancaster, SC (April 2021- and updated in March 2023)
Mom says her perspective has changed after nearly dying of COVID-19, March 10, 2023
When Cierra Chubb looks at her phone, she said she'll often see texts throughout the day from her husband with messages like, "I'm so glad you're here."
That's because at the height of the coronavirus pandemic, Chubb's family did not think the 34-year-old mom of three from Lancaster, South Carolina, would come home to them.
Chubb was one of the hundreds of women in the United States who faced severe complications from COVID-19 during pregnancy.
In Chubb's case, within days of being hospitalized in July 2021, with her pregnancy in distress, doctors made the decision to perform an emergency C-section.
Her son, Myles, was born two weeks premature but healthy. Chubb, though, would go on to spend the next over 100 days hospitalized, with many of those days spent on a ventilator, an ECMO machine and in intensive care.
Chubb's husband, Jamal Chubb, was by his wife's side the entire time. He remembers a conversation he had to have with their oldest child, a daughter named Eden, as a sign of how close Cierra Chubb was to dying.
"Eden was 7 when Cierra got sick and there was a very intimate conversation that she and I had to have," Jamal Chubb recalled to "Good Morning America." "Hey, all the doctors think your mom is going to die, and you need to hear from me before you find it out from anybody else. There are only a few people that believe she's going to live.'"
In the end, Cierra Chubb ended up being one of the lucky ones.
She went home to her husband and three kids in November 2021, five months after being hospitalized. Her return home was the first time she had been reunited with her three children and husband all at once.
"For me personally, looking around our house is like looking at a battlefield almost," Jamal Chubb said. "There was a battle that was fought and won. When I look at Cierra and I look at our children ... it just feels like victory has been won."
The toll COVID-19 took on pregnant women
Saturday, March 11 (2023), marks the third anniversary of the World Health Organization declaring COVID-19 a global pandemic.
Since the start of the pandemic, hundreds of pregnant women in the U.S. have died due to complications from COVID-19, data shows.
In two months alone, August and September 2021, in the United States, more than three dozen pregnant people died of COVID-19, according to the Centers for Disease Control and Prevention. Those deaths came during the height of the Delta variant, which took a particularly hard toll on pregnant women.
Thousands more pregnant women, like Chubb, were hospitalized, often with severe complications, but ultimately survived.
During the pandemic, COVID caused a two-fold risk of admission into intensive care and a 70% increased risk of death for pregnant people, and increases the risk of a stillbirth or delivering preterm, or earlier than 37 weeks, according to the CDC.
Why COVID-19 caused such severe illness in pregnant women became a focus of research over the pandemic, some of which continues to this day.
What doctors do know is that pregnancy causes changes to the immune and respiratory systems that seem to make pregnant women more vulnerable to the disease. The severe lung disease caused by COVID-19 in pregnancy is the major cause of death in pregnancy due to COVID-19 infection.
Research has also shown that pregnant women who are vaccinated have a much lower risk of death and severe complications from COVID-19.
Still, vaccinated pregnant women remain nearly twice as likely to get the virus than those who are vaccinated and not pregnant, data shows.
Moving at the 'speed of gratitude'
Cierra Chubb, who was not vaccinated at the time she contracted COVID-19, said she still struggles with fatigue and has to pace herself doing everyday chores like laundry.
For several weeks, she had supplemental oxygen at home, and for many months she wore a leg brace, but now both of those are gone.
She still has lingering nerve damage in her foot that she said is painful and makes it difficult to walk, but doctors have told her she may see improvement with more time.
Given how sick she was for so many months though, she said she has "improved drastically" and has no long-term health complications from her COVID battle.
"It's been great to do things with my kids that I wasn't doing before, stuff that my daughter is passionate about or helping Langston with video games and watching Myles grow up," she said, referring to her daughter and two sons.
Nearly two years after her own COVID battle, Cierra Chubb said it feels like an "out-of-body experience" to look back on not only her personal struggle but the coronavirus as a whole and the number of people who suffered. More than six million people around the world have died due to COVID-19 to date, according to the World Health Organization.
Jamal Chubb, who spread his wife's story around the world through his viral TikTok updates, said he keeps in touch with people he met along the way, including recently meeting in-person for the first time a woman whose husband was sick with COVID at the same time as Cierra Chubb and passed away.
The Chubbs say they also hear often through social media from people who are hoping for miracles for their loved ones as they say they saw happen with Cierra Chubb.
"There are so many more stories of people who died from COVID than there are people who miraculously made it through COVID," said Jamal Chubb. "So, yes this is a miracle. No, we don't understand it ... Yes, we're holding space for people who lost loved ones, always."
Both Jamal and Cierra Chubb say life for them has returned to a level of normal that they do not take for granted considering the physical and emotional obstacles they've overcome. For many weeks after Cierra Chubb came home, she said their 4-year-old son worried she would leave again and never return.
"For many [normalcy] is an anti-climactic answer, but when you've had a loved one dying and kids not knowing if their mother's coming home, normalcy feels really good," said Jamal Chubb, who continues to share on social media and is now working on a book about his family's journey.
Cierra Chubb said her family has learned to live as though you can go from being sick at home to being near-death in the hospital for five months, as she was. When frustrations arise, she said they have the perspective now to quickly find a solution and move on, adding, "We don't have time to sit and be mad. We're not doing that anymore."
And when Cierra Chubb needs to walk slowly or take a break due to her lingering complications, Jamal Chubb calls it "moving at the speed of gratitude."
"It really slows everything down and causes you to take it all in because there was a battle that we won, and we won it together," he said.
---
The original story on Cierra Chubb was broadcast in August 2021 on Good Morning America: https://www.goodmorningamerica.com/wellness/story/mom-hospitalized-covid-19-complications-vaccine-pregnancy-79365037
and given here:
Mom hospitalized with COVID-19 complications after not getting vaccine during pregnancy, 10 August 2021
A South Carolina woman is fighting for her life in the intensive care unit after contracting COVID-19 while pregnant and giving birth in an emergency c-section.
Cierra Chubb, of Lancaster, South Carolina, tested positive for COVID-19 in late July and was admitted to a local hospital on July 24, her 33rd birthday, according to her husband, Jamal Chubb. The family believes they were exposed to the virus after their 7-year-old daughter attended a summer sports camp where employees later tested positive.
Jamal Chubb, who is vaccinated, did not get COVID-19. However, Cierra Chubb, who wanted to wait until she gave birth to receive a vaccine, and the couple's two oldest children, their 7-year-old daughter and 2-year-old son, all experienced COVID-19 symptoms, according to Jamal Chubb.
"Cierra thought it was just a cold that had been passed around. She didn’t think it was COVID," he told "Good Morning America." "Later down the line, as Cierra’s symptoms worsened, I had her get tested because of how bad her cough was."
Once hospitalized, Cierra was quickly transferred to a larger hospital in Columbia, South Carolina, more than one hour away from the family's home.
Just two days after she was admitted, with her pregnancy in distress, doctors made the decision to perform an emergency c-section, according to Jamal Chubb. The couple's son, Myles, was born on July 26, two weeks before his due date. He weighed five pounds, seven ounces and was healthy, including testing negative for COVID-19, despite his early delivery, according to Jamal Chubb.
Jamal Chubb was allowed to be there for his son's birth, and then had to drive him home alone from the hospital several days later.
"That was the first time Cierra was not in the car with me when we had a newborn sitting in the backseat, making certain he was okay, so I kept putting my hand back in the car seat to make sure he was okay," he said. "It was the most nerve-wracking drive." Shortly after giving birth, Cierra's condition worsened and she was put on a ventilator and then an extracorporeal membrane oxygenation, or ECMO, machine, which removes carbon dioxide from the blood and sends back blood with oxygen to the body, allowing the heart and lungs time to rest and heal.
"That night the doctor called me and told me I could come see her because they weren’t sure if she would survive through the night," said Jamal Chubb. "I went and saw her through the glass window and that was horrible." Cierra Chubb's condition improved but she has remained in a medically-induced coma since early August, according to Jamal Chubb, who has had to take a leave of absence from work in order to care for the couple's three children.
Prisma Health, the company that operates the hospital where Cierra Chubb is being treated, confirmed that she remains in critical condition.
Jamal Chubb said doctors have told him it could take as long as six months for Cierra's organs to be strong enough to operate on their own.
"It’s been hard trying to make a plan for my kids for the future as a ‘single parent’ knowing that my wife is very much alive and fighting for her life, so it’s like holding hope with one hand and planning for the future with the other," he said. "I didn’t sign up to be a single dad. I signed up to build a life with Cierra and my kids together."
Cierra Chubb, a stay-at-home mom who runs her own hand-lettering business, had not yet received the COVID-19 vaccine because she thought she was doing what was best to protect her then-unborn son, according to Jamal Chubb.
"That was her only hesitation in getting vaccinated, was how it was going to affect our son Myles," he said. "She just wanted to protect him at all costs."
Just 16% of pregnant people in the U.S. had received more than one dose of a COVID-19 vaccine as of May, compared to the nearly 58% of Americans ages 12 and up who are fully vaccinated against COVID-19, according to data from the Centers for Disease Control and Prevention.
Earlier this month, the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) -- the nation's two leading health organizations focused on the care of pregnant people -- issued a joint recommendation that all pregnant people should get vaccinated.
The two organizations and other medical experts have cited research showing the vaccine is not dangerous for pregnant people, while complications from COVID-19 are.
Currently, everyone 12 years of age and older, including pregnant people, is eligible to get a COVID-19 vaccination, according to the CDC.
Pregnant people can get the COVID-19 vaccine at any point in their pregnancy, and the vaccine does not need to be spaced from other vaccines, like the flu shot or Tdap booster.
The CDC has shared data showing that pregnant people infected with COVID-19 are at an increased risk for "intensive care unit admission, invasive ventilation, extracorporeal membrane oxygenation, and death," compared to nonpregnant people.
Health experts say that with or without the vaccine, pregnant people need to continue to remain on high alert when it comes to COVID-19 by following safety protocols, including face mask wearing, social distancing and hand washing.
*** New cycles begin ***
Once again considering our fictitious scenario, the Inner Party must face the reality of science: Eventually, sometimes over a period of years, natural immunity resistance renders most viruses sufficiently weak that they do not cause people to visit a hospital. The beauty of the the ‘murder switch’ on their oxygen concentrator/generator is that an entirely pathogen might be construed. Could it be that a new and terrible fungus, rather than a virus, has now evolved? If so, the cycle can begin once more…
*** The Birth of a Deadly Fungus ***
https://www.nytimes.com/2023/03/20/health/candida-auris-us-fungus.html
A deadly fungus that is considered an urgent public health threat by the Centers for Disease Control and Prevention spread at an “alarming rate” during the pandemic, the C.D.C. said on Monday.
The fungus, called Candida auris, preys primarily on older people with weakened immune systems and is particularly dangerous because it resists treatment by common antifungal medications. C. auris was first reported in the United States in 2016, showing up most notably in New York and Illinois, where public health officials hoped they could contain it by rigorous screening and infection control in long-term care facilities and nursing homes.
But over the course of 2021, state and local health departments around the country reported 1,474 clinical cases, about a 200 percent increase from the nearly 500 cases in 2019.
The surge represents a “dramatic increase” in caseload and transmission of C. auris, according to a research paper published Monday in the Annals of Internal Medicine and compiled by researchers at the C.D.C. The fungus is now in half the 50 states, many with just a handful of cases, but with higher concentrations in California, Nevada, Texas and Florida.
The new paper did not include caseloads from 2022. However, a C.D.C. website that tracks the spread of the fungus shows that there were 2,377 infections reported last year, another sharp increase.
Nearly half of patients who contract C. auris die within 90 days, according to the C.D.C. But Dr. Meghan Lyman, a medical officer in the mycotic diseases branch of the C.D.C., said that the agency did not have a good sense of how many deaths to attribute directly to the fungus. The reason is that people who become infected are also dealing with multiple other health challenges, so C. auris can be both a cause of death or something that, along with other poor-health factors, hastens it.
It is likely that the coronavirus pandemic worsened the spread of C. auris, C.D.C. officials said. With attention focused on Covid-19, less emphasis was put on screening for C. auris. Also, the fungus tends to cling to nursing gowns, gloves and other personal protective gear that, under ideal conditions, would be changed frequently but that were reused during the pandemic because of supply shortages. C. auris can also attach to ventilators or other medical equipment.
“We were worried what would happen during Covid,” Dr. Lyman said. She characterized the spread as “concerning but not surprising.”
C. auris is not a particular threat to young healthy people, whose immune systems can fight it off, but can be transported on skin and clothing. Those who contract it can experience typical infection symptoms, like fever and chills that can intensify absent treatment. The fungus commonly strikes older patients, particularly those who have many visits or prolonged visits to health care facilities, where it can be hard to clean or eradicate.
The challenge in treating C. auris stems from the fact that it can be resistant to antifungal medications. During 2020, the research paper found, 86 percent of the germ samples tested by the C.D.C.’s Antimicrobial Resistance Laboratory Network were resistant to a class of drugs known as Azoles.
More concerning to health officials is that 1.2 percent of C. auris samples were resistant that year to a frontline treatment class of drugs called echinocandins. If resistance to echinocandins becomes more common as the germ evolves, C. auris could become extremely difficult, if not impossible, to treat, health officials said.
Dr. Lyman also said that the news is not all bad. Intensive efforts to stop the spread of the germ in New York and Illinois appear to have been effective in containing C. auris within the health care systems in those states — even as the bug rooted elsewhere.
“It’s not a hopeless situation,” Dr. Lyman said.
*** Oh, just one more thing… ***
Overthrowing a strong nation requires its population to accept that its flaws are so deep that it cannot be redeemed. Racial injustice is arguably the weakest point of the history of the United States. Therefore, our fictitious Inner Party would be motivated to demonstrate that racism is not only present, but remains just as prevalent as it ever has been in the US.
As noted earlier, Dr. Mark Melin is currently the West Campus Medical Director of the Wound Healing Institute at Mount Health Fairview (University of Minnesota), which is less than a ten-minute drive from St. Louis Park, MN – the home of the late George Floyd.
According to court testimony, George Floyd went to a hospital twice in March 2020. In the first visit, George Floyd was said (by Derek Chauvin’s defense attorney) to have gone to a hospital for a cut on his hand. (from an exchange available on C-SPAN ( http://www.c-span.org/video/?510411-1/derek-chauvin-trial-death-day-4# )
At approxaimately the 39:00 mark:
Witness Courteney Ross: “We went to the hospital a couple of times in March.”
Chauvin’s Defense Atty: “OK. I understand he was hospitalized for a more extended time period in March. That is the incident I am talking about. I understand he went once because he cut his hand on glass or something and that was a shorter hospital stay...”
Woudn’t it have been logical for George Floyd to go to a nearby hospital which focused on wounds in that circumstance? When George Floyd wounded his hand in March 2020, did he go to the Wound Healing Institute at Mount Health Fairview, the same hospital where Dr. Mark Melin works?
*** Motive of the Inner Party ***
A reasonable question one might have is why a real-world terrorist group might want to inflict harm. Certainly, many different reasons might exist.
Once more, the fiction novel “1984” by George Orwell gives a plausible one.
The book’s antagonist, a character named O’Brien, is questioning the book’s protagonist Winston Smith (in Section 3.3) when Winston guesses that the Inner Party wants totalitarian control over the people stating “You believe that human beings are incapable of governing themselves.” O’Brien responds by inflicting pain upon Winston, calling him “stupid,” and describing the true motive of the Inner Party as follows:
“The Party seeks power for its own sake. We are not interested in the good of others; we are interested solely in power. Not wealth or luxury or long life or happiness; only power, pure power. What pure power means, you will understand presently. We are different from all the oligarchies of the past in that we know what we are doing. All the others, even those who resembled ourselves, were cowards and hypocrites. The German Nazis and Russian Communists came very close to us in their methods, but they never had the courage to recognize their own motives. They pretended, perhaps they even believed, that they had seized power unwillingly and for a limited time, and that just round the corner there lay a paradise where human beings would be free and equal. We are not like that. We know that no one seizes power with the intention of relinquishing it. Power is not a means; it is an end. One does not establish a dictatorship in order to safeguard a revolution; one makes the revolution in order to establish the dictatorship. The object of persecution is persecution. The object of torture is torture. The object of power is power. Do you understand me?”
*** Where do we go from here? ***
“…The story of life is this. Static [clasping ‘Right Hand Love’ and ‘Left Hand Hate’ in opposition to one another]. One hand is always fighting the other hand. And the Left Hand [Hate] is kicking much ass. I mean it looks like the Right Hand Love is finished. But hold on, stop the presses - the Right Hand is coming back! Yeah, he got the Left Hand on the ropes, now! That’s right- yeah! Ooooh, it’s a devastating Right, and Hate is hurt! Down! Ooooh! Left Hand Hate KO’ed by Love!” - Radio Raheem, character from the movie “Do the Right Thing” (second half of Right Hand Love/Left Hand Hate message)
*** End ***